| NAAT Chex TB + Neurocysticercosis | CNS infection panels | 1 working day | Not Available | Whole CSF | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 1-2 ml | PCR |
| SES Acute Encephalitic Syndrome | CNS infection panels | 1 working day | Herpes Simplex Virus 1 & 2;Cytomegalovirus;Varicella Zoster Virus; Human Herpes Virus -6;John Cunningham Virus;JEV;Dengue;West Nile;Enteroviruses;Chikungunya;Rabies;Chandipura;Measels;Mumps;Rubella;Nipah;Mycobacterium tuberculosis;Streptococcus pneumoniae;Haemophilus meningitidis;Cryptococcus neoformans;Toxoplasma gondii | Whole CSF | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 1-2 ml | PCR |
| SES Encephalitis- Outbreak | CNS infection panels | 1 working day | JEV;Dengue;West Nile;Enteroviruses;Chikungunya;Rabies;Chandipura;Measels;Mumps;Rubella;Nipah | Whole CSF | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 1-2 ml | PCR |
| SES Encephalitis- Sporadic | CNS infection panels | 1 working day | Herpes Simplex Virus 1 & 2;Cytomegalovirus;Varicella Zoster Virus; Human Herpes Virus-6;John Cunningham Virus; M. tuberculosis;Streptococcus pneumoniae;Haemophilus meningitidi;Toxoplasma gondi;Cryptococcus neoformans | Whole CSF | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 1-2 ml | PCR |
| SES Meningitis | CNS infection panels | 1 working day | Streptococcus pneumoniae;Haemophilus meningitidis;Mycobacterium tuberculosis;Staphylococcus aureus;Group B Streptococcus; Enterococcus spp;Klebsiella;E.coli;Enterobacter spp;Pseudomonas aeruginosa; Acinetobacter baumannii;Bacteroides fragilis;Leptospira;Cryptococcus neoformans;Aspergillus spp;Candida spp. | Whole CSF | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 1-2 ml | PCR |
| SES Meningitis + ABR | CNS infection panels | 1 working day | Not Available | Whole CSF | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 1-2 ml | PCR |
| SES Pan CNS | CNS infection panels | 1 working day | Streptococcus pneumoniae;Haemophilus meningitidis;Mycobacterium tuberculosis;Staphylococcus aureus;Group B Streptococcus;Enterococci;Klebsiella;E.coli;Enterobacter spp;Pseudomonas aeruginosa; Acinetobacter baumannii;Bacteroides fragilis;Leptospira;Cryptococcus neoformans;Aspergillus spp.;Herpes Simplex Virus 1 & 2;Cytomegalovirus;Varicella Zoster Virus; Human Herpes Virus-6;John Cunningham Virus;Toxoplasma gondii | Whole CSF | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 1-2 ml | PCR |
| SES Pan CNS + ABR | CNS infection panels | 1 working day | Not Available | Whole CSF | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 1-2 ml | PCR |
| SES Fuch's | Eye Infection panels | 1 working day | Herpes Simplex Virus 1&2;Cytomegalovirus;Varicella Zoster Virus;Mycobacterium tuberculosis;Toxoplasma gondii | Aqueous Humor/Vitreous aspirate, Vitreous lavage, Any other eye specimen | Sample collected in 1ml insulin syringe - Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 100 uL | PCR |
| SES Pan Uveitis | Eye Infection panels | 1 working day | Herpes Simplex Virus 1&2;Cytomegalovirus;Varicella Zoster Virus;Chikungunya;Rubella;Dengue;Mycobacterium tuberculosis;Mycobacterium chelonae;Mycobacterium fortuitum;Toxoplasma gondii | Aqueous Humor/Vitreous aspirate, Vitreous lavage, Any other eye specimen | Sample collected in 1ml insulin syringe - Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 100 uL | PCR |
| SES Post Surgical Endophthalmitis | Eye Infection panels | 1 working day | Staphylococcus aureus;Group B Streptococcus; Enterococcus Spp;Coagulase Negative Staphylococcus;Propionibacterium acnce;Pseudomonas aeruginosa;Haemophilus influenzae;Escherichia coli;Klebsiella pneumoniae;Enterobacter aerogenes;Aspergillus Spp.;Candida Spp.;Fusarium Spp | Aqueous Humor/Vitreous aspirate, Vitreous lavage, Any other eye specimen | Sample collected in 1ml insulin syringe - Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 100 uL | PCR |
| SES Traumatic/ Chronic/ Endogenous Endophthalmitis | Eye Infection panels | 1 working day | Staphylococcus aureus;Streptococcus pneumoniae;Group B Streptococcus; Enterococcus Spp;Streptococcus pyogenes;Coagulase Negative Staphylococcus;Propionibacterium acnce;Pseudomonas aeruginosa; Acinetobacter baumanii;Leptospira pathogenic Spp.;Haemophilus meningitidis;Escherichia coli;Klebsiella mirabilis;Salmonella Spp.;Bacteroides fragilis;Aspergillus Spp.;Candida Spp.;Fusarium Spp. | Aqueous Humor/Vitreous aspirate, Vitreous lavage, Any other eye specimen | Sample collected in 1ml insulin syringe - Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 100 uL | PCR |
| SES Viral Retinitis | Eye Infection panels | 1 working day | Herpes Simplex Virus 1&2;Cytomegalovirus;Varicella Zoster Virus | Aqueous Humor/Vitreous aspirate, Vitreous lavage, Any other eye specimen | Sample collected in 1ml insulin syringe - Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 100 uL | PCR |
| BCR-ABL1 MRD | Hemato-oncology | 5 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample to reach laboratory within 24 hours of collection Mandatory Requirement**: - Previous BCR-ABL1 IS Report(s) - Current treatment details - Date of diagnosis of CML disease | Peripheral blood/bone marrow aspirate | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA | Room temperature (refrigerate overnight if necessary) | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | RT-PCR |
| Chimerism [post-engraftment monitoring] | Immunology | 5 working days | 16 STR loci present on different chromosomes are evaluated from patients and donor before transplant and monitor the presence or absence in patient post transplant | Pre-transplant samples for patient and donor: peripheral blood/purified genomic DNA/buccal swabs Po | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; buccal swabs in a sterile tube w | 20-25℃ | Minimum 5ml peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); mi | Fragment Analysis |
| Spinocerebellar ataxia 1 (ATXN1) repeat expansion analysis | Neurology - Movement Disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Fragment analysis |
| Spinocerebellar ataxia 12 (PPP2R2B) repeat expansion analysis | Neurology - Movement Disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Fragment analysis |
| Spinocerebellar ataxia 2 (ATXN2) repeat expansion analysis | Neurology - Movement Disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Fragment analysis |
| Spinocerebellar ataxia 3 (ATXN3) repeat expansion analysis | Neurology - Movement Disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Fragment analysis |
| Spinocerebellar ataxia 6 (CACNA1A) repeat expansion analysis | Neurology - Movement Disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Fragment analysis |
| Spinocerebellar ataxia 7 (ATXN7) repeat expansion analysis | Neurology - Movement Disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Fragment analysis |
| Spinocerebellar ataxia repeat expansion analysis: Any two of (SCA1, SCA2, SCA3, SCA6, SCA7, SCA12) | Neurology - Movement Disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Fragment analysis |
| Spinocerebellar ataxia repeat expansion analysis: SCA1, SCA2, SCA3, SCA6, SCA7,SCA12 | Neurology - Movement Disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Fragment analysis |
| C-MET amplification | Oncology | 7 working days | MET Proto-Oncogene, Receptor Tyrosine Kinase/ HP report should be sent with the sample mandatorily. | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | FISH |
| Comprehensive Tumour Panel (CNVs,SNVs,Short Indels(<10bp), Fusions) + Tumour Mutation Burden | Oncology | 21 working days + 14 working days | Provide histopathological report of patient. Tumor content must be specified. | FFPE blocks | Cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next generation sequencing |
| Comprehensive Tumour Panel (SNVs, Short Indels(<10bp) ) + Tumour Mutation Burden | Oncology | 21 working days + 14 working days | Provide histopathological report of patient. Tumor content must be specified. | FFPE blocks | Cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next generation sequencing |
| Tumour Mutation Burden NGS | Oncology | 14 working days | Provide histopathological report of patient. Tumor content must be specified. | FFPE blocks | Cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next generation sequencing |
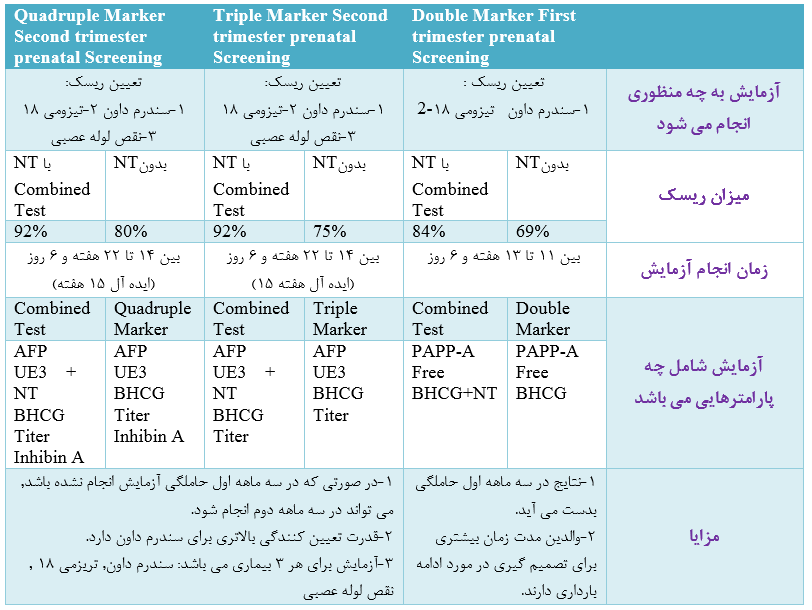
| NIPT | Prenatal | 7 working days | Only singleton pregnancies will be accepted | Maternal peripheral blood in Streck tubes | Peripheral blood in 2 Streck tubes provided in the Lab kit | 6-30℃ | 20ml of maternal peripheral blood in 2 Streck tubes | Next Generation Sequencing |
| PGD for 2 Embryos [NGS] | Prenatal | 14 working days | Pre-PGD passed for 1 variant or multiple Variants in single gene | Day-3 (single cell) or day-5 (few cells) embryo biopsy Note: Day-5 biopsy is preferred | 0.2 ml PCR Tubes from the PGD Kit provided by Lab. Note: Please request for the PGD kit before | -20 to -80℃ (dry ice shipment). Please contact with the Lab prior to performing the biopsy. | Single cell(day-3) or few cells(day-5) embryo biopsy in 2.5 ul transport medium available in the Med | NGS |
| PGD for 3 Embryos [NGS] | Prenatal | 14 working days | Pre-PGD passed for 1 variant or multiple Variants in single gene | Day-3 (single cell) or day-5 (few cells) embryo biopsy Note: Day-5 biopsy is preferred | 0.2 ml PCR Tubes from the PGD Kit provided by Lab. Note: Please request for the PGD kit before | -20 to -80℃ (dry ice shipment). Please contact with the Lab prior to performing the biopsy. | Single cell(day-3) or few cells(day-5) embryo biopsy in 2.5 ul transport medium available in the Med | NGS |
| PGD for 4 Embryos [NGS] | Prenatal | 14 working days | Pre-PGD passed for 1 variant or multiple Variants in single gene | Day-3 (single cell) or day-5 (few cells) embryo biopsy Note: Day-5 biopsy is preferred | 0.2 ml PCR Tubes from the PGD Kit provided by Lab. Note: Please request for the PGD kit before | -20 to -80℃ (dry ice shipment). Please contact with the Lab prior to performing the biopsy. | Single cell(day-3) or few cells(day-5) embryo biopsy in 2.5 ul transport medium available in the Med | NGS |
| PGD for 5 Embryos [NGS] | Prenatal | 14 working days | Pre-PGD passed for 1 variant or multiple Variants in single gene | Day-3 (single cell) or day-5 (few cells) embryo biopsy Note: Day-5 biopsy is preferred | 0.2 ml PCR Tubes from the PGD Kit provided by Lab. Note: Please request for the PGD kit before | -20 to -80℃ (dry ice shipment). Please contact with the Lab prior to performing the biopsy. | Single cell(day-3) or few cells(day-5) embryo biopsy in 2.5 ul transport medium available in the Med | NGS |
| PGD per Embryo [NGS] | Prenatal | 14 working days | Pre-PGD passed for 1 variant or multiple Variants in single gene | Day-3 (single cell) or day-5 (few cells) embryo biopsy Note: Day-5 biopsy is preferred | 0.2 ml PCR Tubes from the PGD Kit provided by Lab. Note: Please request for the PGD kit before | -20 to -80℃ (dry ice shipment). Please contact with the Lab prior to performing the biopsy. | Single cell(day-3) or few cells(day-5) embryo biopsy in 2.5 ul transport medium available in the Med | NGS |
| Pre-PGD for parents and proband (Max 3 samples) - More than 1 variant or multiple Variants in single | Prenatal | 21 working days | All 3 samples(when available) or at least the samples of prospective parents will be processed | Peripheral blood | EDTA anticoagulated peripheral blood | 20-25℃ | Minimum 3ml of peripheral blood | NGS |
| NAAT CheX Dengue Virus | Systemic Infection Panels | 1 working day | Not Available | Whole Blood (Peripheral Blood), Bronchoalveolar Lavage (BAL), Any sterila body fluid | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| SES Antibiotic Resistance Markers (ABR) | Systemic Infection Panels | 1 working day | ESBL – Detects Genes that confer Resistance to 3rd & 4th Generation Cephalosporins; Carbapenem – Detects both Betalactamases & MetalloBetalactamases; NDM-1 – Detects New Delhi Metallo betalactamase; Van A- Detects resistance to Vancomycin & Teicoplanin; Van B- Detects resistance to Vancomycin (Teicoplanin sensitive);Methicillin A– Detects resistance to Methicillin | Whole Blood (Peripheral Blood), Bronchoalveolar Lavage (BAL), Tissue, any sterile body fluid | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| SES Community Acquired Pneumonia (CAP) | Systemic Infection Panels | 1 working day | Staphylococcus aureus;Streptococcus pneumoniae;Klebsiella pneumoniae;Haemophilus influenzae;Pseudomonas aeruginosa; Acinetobacter baumanii;Salmonella spp.;Mycoplasma pneumonia;Chlamydia pneumonia; P. jiroveci;Cytomegalovirus;Adenovirus;Influenza A, B,C; Parainfluenza 1,2,3,4;RSV A and B;Rhinoviruses;Enteroviruses;Coronaviruses OC43, 229E, NL63, HKU1;Human-Metapneumoviruses;Parechoviruses;SARS | Whole Blood (Peripheral Blood), Bronchoalveolar Lavage (BAL), Tracheal aspirate | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| SES MDR Tuberculosis | Systemic Infection Panels | 1 working day | Rifampicin Resistance; IHN Resistance | Wound Swab, Bronchoalveolar Lavage (BAL), Tissue, any sterile body fluid | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| SES Mycobacteria | Systemic Infection Panels | 1 working day | Mycobacterium tuberculosis; Mycobacterium chelonae; Mycobacterium fortuitum; Mycobacterium spp | Wound Swab, Bronchoalveolar Lavage (BAL), Tissue, any sterile body fluid | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| SES Post Transplant/ Febrile Neutropenia + ABR | Systemic Infection Panels | 1 working day | Not Available | Whole Blood (Peripheral Blood), Bronchoalveolar Lavage (BAL), Tissue, any sterile body fluid | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| SES Post Transplant/ Febrile Neutropenia/ Pneumonia | Systemic Infection Panels | 1 working day | Staphylococcus aureus; Streptococcus B Streptococcus; Enterococcus spp; Mycobacterium tuberculosis; Klebsiella influenzae; Neisseria meningitidis; Pseudomonas aeruginosa; Acinetobacter baumanii; Escherichia coli; Salmonella spp.;Bacteroides fragilis; Leptospira pathogenic spp. Aspergillus spp.; Candida Spp.; Cryptococcus neoformans; Herpes Simplex Virus 1&2;Cytomegalovirus;Varicella Zoster Virus; Human Herpes Virus 6;Adeno Virus; John Cunningham Virus; BK Virus; Epstein Barr Virus | Whole Blood (Peripheral Blood), Bronchoalveolar Lavage (BAL), Tissue, any sterile body fluid | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| SES Respiratory Viral | Systemic Infection Panels | 1 working day | Cytomegalovirus; Adenovirus; Influenza A, B,C; Parainfluenza 1,2,3,4;RSV A and B;Rhinoviruses;Enteroviruses;Coronaviruses OC43,229E, NL63, HKU1;Human-Metapneumoviruses;Parechoviruses;SARS | Naso Pharengeal wash, Bronchoalveolar Lavage (BAL)/Tracheal aspirate | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| SES Sepsis | Systemic Infection Panels | 1 working day | Staphylococcus aureus; Streptococcus pneumoniae; Streptococcus pyogenes; Group B Streptococcus; Enterococcus spp; Klebsiella pneumoniae; Enterobacter aerogenes; Proteus mirabilis; Haemophilus influenzae; Neisseria meningitidis; Pseudomonas aeruginosa; Acinetobacter baumanii; Escherichia coli; Salmonella spp.;Bacteroides fragilis; Leptospira pathogenic spp.;Aspergillus spp.; Candida spp. | Whole Blood (Peripheral Blood), Bronchoalveolar Lavage (BAL), Tissue, any sterile body fluid | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| SES Sepsis + ABR | Systemic Infection Panels | 1 working day | Not Available | Whole Blood (Peripheral Blood), Bronchoalveolar Lavage (BAL), Tissue, any sterile body fluid | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| SES Transplant Viral | Systemic Infection Panels | 1 working day | Herpes Simplex Virus 1&2;Cytomegalovirus;Varicella Zoster Virus; Human Herpes Virus 6;Adeno Virus; John Cunningham Virus; Epstein Barr Virus | Whole Blood (Peripheral Blood), Bronchoalveolar Lavage (BAL), Any sterile body fluid | Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 2-3 ml | PCR |
| Prenatal sanger variant analysis [1 variant] (Primers available) | Additional options for testing | 12 working days | Detailed clinical and family history is mandatory for processing this test | Chorionic villus sample (CVS)/amniotic fluid/fetal DNA | CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic;Amniotic fluid in a sterile f | 20-25℃; CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency; minimum 1 microg | Sanger sequencing |
| Prenatal sanger variant analysis [2 variant] (Primers available) | Additional options for testing | 12 working days | Detailed clinical and family history is mandatory for processing this test | Chorionic villus sample (CVS)/amniotic fluid/fetal DNA | CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic;Amniotic fluid in a sterile f | 20-25℃; CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency; minimum 1 microg | Sanger sequencing |
| Prenatal sanger variant analysis [3 variants] | Additional options for testing | 28 working days | Detailed clinical and family history is mandatory for processing this test | Chorionic villus sample (CVS)/amniotic fluid/fetal DNA | CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic; Amniotic fluid in a sterile f | 20-25℃; CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency; minimum 1 microgram | Sanger sequencing |
| Sanger validation [3 variants] | Additional options for testing | 28 working days | Detailed clinical and family history is mandatory for processing this test | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Sanger sequencing |
| Cardiac channelopathy gene panel | Cardiology | 21 working days | ABCC9, AKAP9, ALG10, ANK2, CACNA1C, CACNA1D, CACNB2, CALM1, CALM2, CASQ2, CAV3, DPP6, GATA4, GJA5, GNAI2, GPD1L, HCN4, KCNA5, KCND3, KCNE1, KCNE2, KCNE3, KCNH2, KCNJ2, KCNJ5, KCNJ8, KCNQ1, NKX2-5, NPPA, NUP155, RANGRF, RYR2, SCN10A, SCN1B, SCN2B, SCN3B, SCN4B, SCN5A, SNTA1, TRDN, TRPM4 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃; CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Cardiomyopathy gene panel | Cardiology | 21 working days | AARS2, ABCC9, ACAD9, ACADVL, ACTA1, ACTC1, ACTN2, AGK, AGL, ALMS1, ANK2, ANKRD1, ANO5, BAG3, BIN1, BRAF, CALR3, CASQ2, CAV3, CFL2, CHKB, CHRM2, COX15, CPT1A, CPT2, CRYAB, CSRP3, CTF1, CTNNA3, DES, DMD, DNAJC19, DNM2, DOLK, DPP6, DSC2, DSG2, DSG3, DSP, DTNA, DYSF, EMD, EYA4, FHL1, FHL2, FHOD3, FKTN, FLNC, FOXRED1, FXN, GAA, GATAD1, GJA1, GJA5, GLA, GLB1, GNE, GUSB, HCN4, HFE, HRAS, ILK, ISCU, JPH2, JUP, KBTBD13, KCNA5, KCND3, KCNJ8, KLHL9, KRAS, LAMA4, LAMP2, LDB3, LMNA, LZTR1, MAP2K1, MAP2K2, MEGF10, MIB1, MSTN, MTM1, MTO1, MYBPC1, MYBPC3, MYF6, MYH2, MYH6, MYH7, MYL2, MYL3, MYLK2, MYOT, MYOZ2, MYPN, NEB, NEBL, NEXN, NF1, NOS1AP, NPPA, NRAS, OBSCN, PABPN1, PDLIM3, PKP2, PLEC, PLN, PRDM16, PRKAG2, PSEN1, PSEN2, PTPN11, PTRF, RAF1, RANGRF, RBM20, RIT1, RYR2, SCN10A, SCN5A, SCNN1B, SCNN1G, SCO2, SDHA, SEPN1, SGCD, SGCG, SHOC2, SLC22A5, SLC25A20, SLC25A4, SOS1, SRL, TAZ, TBX20, TCAP, TGFB3, TMEM43, TMEM70, TMPO, TNNC1, TNNI3, TNNI3K, TNNT2, TPM1, TSFM, TTN, TTR, VCL, VCP, XK | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Cardiomyopathy predisposition - MYBPC3 (25bp deletion) by PCR-gel | Cardiology | 7 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | PCR |
| Clopidogrel dosage CYP2C19*2 & CYP2C19*3 | Cardiology | 3 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | RT-PCR |
| Statin induced myopathy predisposition SLCO1B1 p.(Val174Ala) by RT-PCR | Cardiology | 7 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | RT-PCR |
| Warfarin dosage-VKORC1 (c.-1639 G>A), CYP2C9*2,CYP2C9*3,CYP2C9*13 by RT-PCR | Cardiology | 7 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | RT-PCR |
| Connective tissue disorder gene panel | Connective Tissue Disorders | 21 working days | ABCC6, ACTA2, ACVR1, ADAMTS10, ADAMTS2, ADAMTSL2, AGPS, ALDH18A1, ALPL, ARSE, ATP6V0A2, ATP7A, B3GALT6, B4GALT7, BMP1, CA2, CANT1, CBS, CHST14, CLCN7, COL10A1, COL11A1, COL11A2, COL1A1, COL1A2, COL2A1, COL3A1, COL4A3, COL4A4, COL4A5, COL5A1, COL5A2, COL9A1, COL9A2, COL9A3, COMP, CRTAP, DDR2, DSE, DYNC2H1, EBP, EFEMP2, ELN, EVC, EVC2, FBLN5, FBN1, FBN2, FGFR1, FGFR3, FKBP10, FKBP14, FLCN, FLNA, FLNB, GDF5, GNPAT, HSPG2, IFITM5, IFT122, IFT43, IFT80, IHH, LBR, LIFR, LRP5, LTBP2, LTBP4, MYH11, MYLK, NEK1, NOTCH1, NPR2, NSDHL, OCRL, OSTM1, P3H1, PAPSS2, PEX7, PIEZO2, PKD2, PLEKHM1, PLOD1, PLOD2, PLOD3, PPIB, PRDM5, PTH1R, PYCR1, RIN2, RMRP, RUNX2, SERPINF1, SERPINH1, SKI, SLC26A2, SLC2A10, SLC35D1, SLC39A13, SMAD3, SMAD4, SMARCAL1, SNX10, SOX9, SP7, SPARC, TCIRG1, TGFB1, TGFB2, TGFB3, TGFBR1, TGFBR2, TMEM38B, TNFRSF11A, TNFSF11, TNXB, TRAPPC2, TRIP11, TRPS1, TRPV4, TTC21B, WDR35, WISP3, WNT1, ZNF469 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Cutis-laxa gene panel | Connective Tissue Disorders | 21 working days | ALDH18A1, ATP6VA2, ATP6V1A, ATP6V1E1, ATP7A, EFEMP2, ELN, FBLN5, LTBP4, PYCR1, RIN2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Ehler Danlos syndrome gene panel | Connective Tissue Disorders | 21 working days | ADAMTS2, ATP7A, B3GALT6, B4GALT7, C1R, CHST14, COL1A1, COL1A2, COL3A1, COL5A1, COL5A2, DSE, FKBP14, FLNA, PLOD1, SLC39A13, TNXB, ZNF469 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Ehlers-Danlos syndrome type VI (PLOD1) deletion/duplication analysis | Connective Tissue Disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Marfan syndrome (FBN1) gene analysis | Connective Tissue Disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Acute intermittent porphyria - HMBS gene analysis | Dermatology | 21 working days | HMBS | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Ectodermal dysplasia gene panel | Dermatology | 21 working days | CDH3, DLX3, EDA, EDAR, EDARADD, EVC, EVC2, GJB6, GRHL2, HOXC13, KDF1, KREMEN1, KRT74, KRT85, MBTPS2, MSX1, NFKBIA, NLRP1, ORAI1, PKP1, PVRL1, PVRL4, TP63, TWIST2, WNT1A | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Epidermolysis bullosa gene panel | Dermatology | 21 working days | CD151, COL17A1, COL7A1, DSP, DST, EXPH5, FERMT1, ITGA3, ITGA6, ITGB4, KRT14, KRT5, LAMA3, LAMB3, LAMC2, MMP1, PKP1, PLEC, TGM5 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Harlequin ichthyosis (ABCA12) gene analysis | Dermatology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Icthyosis gene panel | Dermatology | 21 working days | ABCA12, ABHD5, ALDH3A2, ALOX12B, ALOXE3, AP1S1, CASP14, CDSN, CERS3, CLDN1, CSTA, CYP4F22, DSG1, DSP, EBP, FLG, GJB2, GJB3, GJB4, KRT1, KRT1, KRT2, LIPN, LOR, NIPAL4, PHGDH, PHYH, PNPLA1, POMP, PSAT1, SLC27A4, SLURP1, SNAP29, SPINK5, ST14, STS, TGM1, TGM5 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Oculocutaneous albinism gene panel | Dermatology | 21 working days | C10orf11, MC1R, OCA2, SLC24A5, SLC45A2, TYR, TYRP1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Sjogren-Larsson syndrome (ALDH3A2) gene analysis | Dermatology | 21 working days | Provide details of immunological involvement and clinical history especially pertaining to skin, joints, bones and eye | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Xeroderma pigmentosum gene panel | Dermatology | 21 working days | DDB2, ERCC2, ERCC3, ERCC4, ERCC5, POLH, XPA, XPC | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Androgen receptor (AR) deletion/duplication analysis | Endocrinology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Androgen receptor (AR) gene analysis | Endocrinology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Congenital adrenal hyperplasia CYP21A2 (21-0H) deletion/duplication analysis | Endocrinology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Congenital adrenal hyperplasia CYP21A2 (21-0H) gene analysis | Endocrinology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Congenital adrenal hyperplasia due to 3-beta-hydroxysteroid dehydrogenase 2 deficiency (HSD3B2) gene | Endocrinology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Congenital adrenal hyperplasia due to 3-beta-hydroxysteroid dehydrogenase 2 deficiency (HSD3B2) gene | Endocrinology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Congenital hypopituitarism gene panel | Endocrinology | 21 working days | GLI2, GLI3, HESX1, LHX3, LHX4, OTX2, POU1F1, PROP1, SOX3 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hereditary pancreatitis gene panel | Endocrinology | 21 working days | CFTR, CTRC, PRSS1, SPINK1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hypercholesterolemia gene panel | Endocrinology | 21 working days | ABCA1, ABCG5, ABCG8, APOA1, APOA2, APOA5, APOB, APOC2, APOC3, APOE, CETP, EPHX2, GHR, GPIHBP1, ITIH4, LDLR, LDLRAP1, LIPC, LPL, PCSK9, PPP1R17, SLCO1B1, SREBF2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Kallmann syndrome gene panel | Endocrinology | 21 working days | FGFR1, KAL1, PROK2, PROKR2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Leptin deficiency (LEP) gene analysis | Endocrinology | 21 working days | LEP | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Maturity-onset diabetes of the young (MODY) & neonatal diabetes gene panel | Endocrinology | 21 working days | ABCC8, AKT2, APPL1, BLK, CEL, CISD2, EIF2AK3, FOXP3, GCK, GLIS3, GLUD1, HADH, HNF1A, HNF1B, HNF4A, IER3IP1, INS, INSR, KCNJ11, KLF11, MNX1, NEUROD1, NKX2-2, NKX6- 1, PAX4, PDX1, PTF1A, RFX6, SLC2A2, WFS1, ZFP57 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Monogenic and syndromic obesity gene panel | Endocrinology | 21 working days | ALMS1, ARL6, BBS1, BBS10, BBS12, BBS2, BBS4, BBS5, BBS7, BBS9, CEP290, CREBBP, CUL4B, DYRK1B, EP300, GNAS, INPP5E, KSR2, LEP, LEPR, MAGEL2, MC3R, MC4R, MEGF8, MKKS, MKS1, NR0B2, NTRK2, PCNT, PCSK1, PHF6, POMC, PPARG, PYY, RAB23, RPS6KA3, SDCCAG8, SIM1, TBX3, TMEM67, TRIM32, TTC8, VPS13B, WDPCP | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Deafness gene panel | ENT | 21 working days | ACTB, ACTG1, ADCY1, ADGRV1, AIFM1, ATP6V1B1, BCS1L, BDP1, BSND, BTD, CABP2, CACNA1D, CCDC50, CD164, CDC14A, CDH23, CEACAM16, CIB2, CISD2, CLDN14, CLIC5, CLPP, CLRN1, COCH, COL11A1, COL11A2, COL2A1, COL4A3, COL4A4, COL4A5, COL4A6, COL9A1, COL9A2, COL9A3, CRYM, DCDC2, DFNA5, DFNB31, DFNB59, DIABLO, DIAPH1, DIAPH3, DMXL2, DNMT1, DSPP, EDN3, EDNRB, ELMOD3, EPS8, EPS8L2, ESPN, ESRRB, EYA1, EYA4, FAM189A2, FAM65B, FGF3, FOXI1, GATA3, GIPC3, GJB1, GJB2, GJB3, GJB4, GJB6, GPSM2, GRHL2, GRXCR1, GRXCR2, HARS, HARS2, HGF, HOMER2, HSD17B4, ILDR1, JAG1, KARS, KCNE1, KCNJ10, KCNQ1, KCNQ4, LARS2, LHFPL5, LHX3, LOXHD1, LRTOMT, MARVELD2, MCM2, MET, MIR96, MITF, MSRB3, MYH14, MYH9, MYO15A, MYO1A, MYO1C, MYO1F, MYO3A, MYO6, MYO7A, NARS2, NF2, OSBPL2, OTOA, OTOF, OTOG, OTOGL, P2RX2, PAX3, PCDH15, PDZD7, PEX7, PHYH, PNPT1, POU3F4, POU4F3, PRPS1, PTPRQ, RDX, S1PR2, SERPINB6, SIX5, SLC17A8, SLC22A4, SLC26A4, SLC26A5, SLITRK6, SMPX, SNAI2, SOX10, SOX2, STRC, SYNE4, TBC1D24, TECTA, TIMM8A, TJP2, TMC1, TMEM132E, TMIE, TMPRSS3, TMPRSS5, TNC, TPRN, TRIOBP, TSPEAR, USH1C, USH1G, USH2A, WBP2, WFS1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Mondini defect (SLC26A4) gene analysis | ENT | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Waardenburg syndrome gene panel | ENT | 21 working days | EDN3, EDNRB, MITF, PAX3, SNAI2, SOX10, TYR | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Alagille syndrome gene panel | Gastroenterology | 21 working days | JAG1, NOTCH2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Congenital hepatic fibrosis gene panel | Gastroenterology | 21 working days | AHI1, ANKS6, ARL13B, ARL6, B9D1, B9D2, BBS1, BBS10, BBS12, BBS2, BBS4, BBS5, BBS7, BBS9, C5orf42, CC2D2A, CEP164, CEP290, CEP41, EVC, EVC2, GLIS2, IFT122, IFT80, INPP5E, INVS, IQCB1, KIF7, MKKS, MKS1, NEK8, NPHP1, NPHP3, NPHP4, OFD1, PKD1, PKD2, PKHD1, RPGRIP1L, TCTN1, TCTN2, TCTN3, TMEM138, TMEM216, TMEM231, TMEM237, TMEM67, TRIM32, TTC21B, TTC8, WDR19, ZNF423 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Gilbert syndrome (UGT1A1) gene analysis (only point mutation analysis) | Gastroenterology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hemochromatosis gene panel | Gastroenterology | 21 working days | BMP2, FTH1, HAMP, HFE, HFE2, SLC40A1, TFR2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Polycystic liver disease gene panel | Gastroenterology | 21 working days | ALG8, GANAB, LRP5, PKHD1, PRKCSH, SEC63 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Progressive familial intrahepatic cholestasis gene panel | Gastroenterology | 21 working days | ABCB11, ABCB4, AKR1D1, ATP8B1, JAG1, NOTCH2, NR1H4, SLC25A13, TJP2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Progressive familial intrahepatic cholestasis-3 (ABCB4) deletion/duplication analysis | Gastroenterology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Tyrosinemia gene analysis | Gastroenterology | 21 working days | FAH, HPD, TAT | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| UGT1A1 repeat analysis | Gastroenterology | 14 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Fragment analysis |
| Wilson disease (ATP7B) deletion/duplication analysis | Gastroenterology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Wilson disease (ATP7B) gene analysis | Gastroenterology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Alpha thalassemia (HBA1 & HBA2) deletion/duplication analysis | Hematology | 14 working days | Not Available | Peripheral blood/purified genomic DNA (RNAse treated)/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Alpha thalassemia gene analysis (HBA1 & HBA2) | Hematology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Sanger sequencing |
| Aplastic anemia gene panel | Hematology | 21 working days | ACD, BRCA1, BRCA2, BRIP1, DKC1, ERCC4, FANCA, FANCB, FANCC, FANCD2, FANCE, FANCF, FANCG, FANCI, FANCL, FANCM, GATA1, NBN, NHP2, NOP10, PALB2, PARN, PRF1, RAD51C, RPL11, RPL15, RPL26, RPL35A, RPL5, RPS10, RPS19, RPS24, RPS26, RPS28, RPS29, RPS7, RTEL1, SBDS, SLX4, TERT, TINF2, TSR2, UBE2T, WRAP53 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Beta thalassemia (HBB) deletion/duplication analysis | Hematology | 14 working days | Not Available | Peripheral blood/purified genomic DNA (RNAse treated)/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Beta thalassemia [HBB] gene analysis | Hematology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Bone marrow failure syndrome gene panel | Hematology | 21 working days | AK2, ANKRD26, ATR, BRCA1, BRCA2, BRIP1, CEBPA, CECR1, CSF3R, CTC1, DDX41, DKC1, DNAJC21, ELANE, ERCC4, ETV6, FANCA, FANCB, FANCC, FANCD2, FANCE, FANCF, FANCG, FANCI, FANCL, FANCM, G6PC3, GATA1, GATA2, GFI1, GFI1B, HAX1, JAGN1, LIG4, MPL, NBN, NHP2, NOP10, PALB2, PARN, PAX5, RAB27A, RAD51, RAD51C, RMRP, RPL11, RPL15, RPL19, RPL23, RPL26, RPL27, RPL31, RPL35A, RPS10, RPS15, RPS19, RPS24, RPS26, RPS27, RPS27A, RPS28, RPS29, RPS7, RTEL1, RUNX1, SAMD9, SAMD9L, SBDS, SLX4, SRP72, TAZ, TCIRG1, TERC, TERT, TINF2, TP53, TSR2, UBE2T, USB1, VPS13B, VPS45, WAS, WRAP53 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| CD34+ Stem cell Enumeration (CD45, CD34, 7AAD) | Hematology | 4 hours | Provide detailed clinical history along with CBC reports | Bone marrow/ Peripheral blood in EDTA /Harvest Sample | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 2-8℃ | 2 mL | Flowcytometry |
| Congenital afibrinogenemia gene panel | Hematology | 21 working days | FGA, FGB, FGG | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Congenital dyserythropoietic anemia gene panel | Hematology | 21 working days | C15orf41, CDAN1, COX4I2, GATA1, KIF23, KLF1, SEC23B | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Diamond blackfan anemia gene panel | Hematology | 21 working days | GATA1, RPL11, RPL15, RPL26, RPL27, RPL35A, RPL5, RPS10, RPS19, RPS24, RPS26, RPS27, RPS28, RPS29, RPS7, TSR2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Dyskeratosis congenita gene panel | Hematology | 21 working days | ACD, CTC1, DKC1, NHP2, NOP10, PARN, RTEL1, TERT, TINF2, WRAP53 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Factor V Leiden (F5) mutation analysis (exon 10) | Hematology | 7 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Sanger sequencing |
| Factor VII deficiency (F7) gene analysis | Hematology | 21 working days | AK2, ANKRD26, ATR, BRCA1, BRCA2, BRIP1, CEBPA, CECR1, CSF3R, CTC1, DDX41, DKC1, DNAJC21, ELANE, ERCC4, ETV6, FANCA, FANCB, FANCC, FANCD2, FANCE, FANCF, FANCG, FANCI, FANCL, FANCM, G6PC3, GATA1, GATA2, GFI1, GFI1B, HAX1, JAGN1, LIG4, MPL, NBN, NHP2, NOP10, PALB2, PARN, PAX5, RAB27A, RAD51, RAD51C, RMRP, RPL11, RPL15, RPL19, RPL23, RPL26, RPL27, RPL31, RPL35A, RPS10, RPS15, RPS19, RPS24, RPS26, RPS27, RPS27A, RPS28, RPS29, RPS7, RTEL1, RUNX1, SAMD9, SAMD9L, SBDS, SLX4, SRP72, TAZ, TCIRG1, TERC, TERT, TINF2, TP53, TSR2, UBE2T, USB1, VPS13B, VPS45, WAS, WRAP53 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Fanconi anemia gene panel | Hematology | 21 working days | BRCA1, BRCA2, BRIP1, ERCC4, FANCA, FANCB, FANCC, FANCD2, FANCE, FANCF, FANCG, FANCI, FANCL, FANCM, MAD2L2, PALB2, RAD51, RAD51C, SLX4, UBE2T, XRCC2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Fanconi anemia of complementation group A (FANCA) deletion/duplication analysis | Hematology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Fanconi's Anemia | Hematology | 15 working days | Not Available | Peripheral Blood | Sodium heparin-Green top | 20-25℃ | Minimum 4 ml peripheral blood | Cytogenetics/Karyotyping |
| G6PD gene sequencing | Hematology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Haemophilia (F8 & F9) gene panel | Hematology | 21 working days | F8, F9 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Haemophilia A (F8) gene analysis (analysis of the F8 inversion is not included) | Hematology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Haemophilia A (F8) intron 22 inversion | Hematology | 10 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | PCR |
| Hemophagocytic lymphohistiocytosis (HLH) gene panel | Hematology | 21 working days | AP3B1, BLOC1S6, CD27, ITK, LYST, PRF1, RAB27A, SH2D1A, SLC7A7, STX11, STXBP2, UNC13D, XIAP | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hemophagocytic lymphohistiocytosis deletion/duplication analysis | Hematology | 14 working days | PRF1, STK11, UNC13D | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Hereditary elliptocytosis gene panel | Hematology | 21 working days | EPB41, SLC4A1, SPTA1, SPTB | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hereditary Hemolytic Anemia Panel (For RBC membrane disorders and Enzymopathies) | Hematology | 21 working days | ABCG5, ABCG8, AK1, ALDOA, ANK1, C15orf41, CDAN1, EPB41, EPB42, G6PD, GATA1, GCLC, GPI, GPX1, GSR, GSS, HK1, KIF23, KLF1, NT5C3A, PFKM, PGK1, PIEZO1, PKLR, RHAG, SEC23B, SLC2A1, SLC4A1, SPTA1, SPTB, TPI1, XK | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hereditary spherocytosis gene panel | Hematology | 21 working days | ANK1, EPB42, SLC4A1, SPTA1, SPTB | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Iron-refractory iron deficiency anemia (TMPRSS6) gene analysis | Hematology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Methemoglobinemia (CYB5R3) gene analysis | Hematology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| MTHFR gene analysis - 2 exons (5 & 8) | Hematology | 10 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Sanger sequencing |
| Protein S deficiency (PROS1 gene deletion/duplication analysis ) | Hematology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Sickle cell anemia (HBB) gene analysis (exon 1) | Hematology | 10 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Sanger Sequencing |
| Sideroblastic anaemia gene panel | Hematology | 21 working days | ABCB7, ALAS2, GLRX5, PUS1, SLC25A38, TRNT1, YARS2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Von Willebrand disease (VWF) gene analysis | Hematology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Wiskott Aldrich syndrome (WAS) gene analysis | Hematology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Myeloproliferative neoplasm (MPN) reflex panel NGS | Hemato-oncology | 8 working days | JAK2 Sanger sequencing for exons 12 & 14 if negative MPL Sanger sequencing for exon 10 if negative CALR Fragment analysis of exon 9 | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next generation Sequencing |
| Acute Leukemia Classifier Panel - Flowcytometry | Hemato-oncology | 2 working days | Appropriately labelled air-dried and unstained Bone marrow aspirate smears and Peripheral blood smears must accompany every specimen. | Peripheral blood along with bone marrow aspirate in EDTA, Peripheral blood can be accepted if blasts/ | Bone marrow smears on slides; bone marrow aspirate in EDTA; EDTA anticoagulated peripheral blood | 2-8℃ | Minimum of 2 bone marrow smears; minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | Flowcytometry |
| Acute Leukemia Screen Panel - Flowcytometry | Hemato-oncology | 2 working days | Appropriately labelled air-dried and unstained Bone marrow aspirate smears and Peripheral blood smears must accompany every specimen. | Peripheral blood along with bone marrow aspirate in EDTA. Peripheral blood can be accepted if blasts/a | Bone marrow smears on slides; bone marrow aspirate in EDTA; EDTA anticoagulated peripheral blood | 2-8℃ | Minimum of 2 bone marrow smears; minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | Flowcytometry |
| ALL risk stratification gene panel - B-ALL | Hemato-oncology | 14 working days | ABL1, CDKN2A, CREBBP, ETV6, FLT3, IKZF1, JAK2, KDM6A, KRAS, MLL2, NRAS, PTEN, TP53 Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| ALL risk stratification gene panel - T-ALL | Hemato-oncology | 14 working days | DNMT3A, HRAS, KRAS, NOTCH1, NRAS, PHF6, PTEN, RUNX1 Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| AML risk stratification gene panel | Hemato-oncology | 14 working days | ASXL1, BRAF, CEBPA, CUX1, DNMT3A, ETV6/TEL, EZH2, FLT3, GATA1, GATA2, HRAS, IDH1, IDH2, JAK2, KIT (c-KIT), KRAS, MLL, NPM1, NRAS, PDGFRA, PHF6, PTPN11, RUNX1, SETBP1, STAG2, TET2, TP53, WT1, ZRSR2 Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| BCR-ABL qualitative gene fusion analysis (Major,Minor & Micro) | Hemato-oncology | 4 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample to reach laboratory within 24 hours of collection | Peripheral blood/bone marrow aspirate | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA | Room temperature (refrigerate overnight if necessary) | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | RT-PCR |
| BCR-ABL quantitative (International Scale) gene fusion analysis | Hemato-oncology | 5 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample to reach laboratory within 24 hours of collection | Peripheral blood/bone marrow aspirate | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA | Room temperature (refrigerate overnight if necessary) | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | RT-PCR |
| BCR-ABL quantitative gene fusion analysis (Major,Minor & Micro) | Hemato-oncology | 4 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample to reach laboratory within 24 hours of collection | Peripheral blood/bone marrow aspirate | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA | Room temperature (refrigerate overnight if necessary) | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | RT-PCR |
| CEL/diagnostic and prognostic gene panel | Hemato-oncology | 14 working days | PDGFRA and KIT mutations Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| Chronic Lymphoid Leukemia Panel - Flowcytometry | Hemato-oncology | 2 working days | Appropriately labelled air-dried and unstained Bone marrow aspirate smears and Peripheral blood smears must accompany every specimen. | Peripheral blood along with bone marrow aspirate in EDTA. Peripheral blood can be accepted if blasts/ | Bone marrow smears on slides; bone marrow aspirate in EDTA; EDTA anticoagulated peripheral blood | 2-8℃ | Minimum of 2 bone marrow smears; minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | Flowcytometry |
| Chronic myeloproliferative disorder gene panel (CMPD) | Hemato-oncology | 14 working days | ABL1, CALR, CBL, CBLB, CBLC, CSF3R, JAK2, KIT, MPL, PDGFRA Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| CLL prognostication/Risk stratification gene panel | Hemato-oncology | 14 working days | MYD88, NOTCH1, SF3B1, TP53 Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| CML/CNL(atypical) prognostication gene panel | Hemato-oncology | 14 working days | ASXL1, CBL, CBLB, CBLC, CSF3R, DNMT3A, JAK2, SETBP1, NRAS, KRAS Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| CMML risk stratification gene panel | Hemato-oncology | 14 working days | ASXL1, CBLC, SETBP1, TET2, EZH2, SF3B1, ZRSR2, RUNX1, TP53 Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| Comprehensive ALL Panel (FISH,Karyotyping,MLPA,NGS,RT-PCR) | Hemato-oncology | 21 working days | MGM576-Karyotyping- bone marrowMGM174-BCR-ABL quantitative (International Scale) gene fusion analysis (RT-PCR);MGM1060-Multiplex RT-PCR panel for Leukemia(RT-PCR);MGM461-AML/MDS FISH for C-MYC amplifications/trisomy8(FISH);MGM499-Comprehensive leukemia panel - 57 genes(NGS);MGM1139-iAMP21 by FISH(FISH);MGM1144-TCR-alpha and TCR-delta(FISH) | Bone marrow/ Peripheral blood in EDTA, Bone marrow/ Peripheral blood in heparin | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA, Bone marrow/ Peripheral blood in | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | FISH,Karyotyping,MLPA,Next Generation Sequencing,RT-PCR |
| Comprehensive leukemia panel - 57 genes | Hemato-oncology | 14 working days | ABL1, ASXL1, ATM, ATRX, BCOR, BRAF, CALR, CBL, CBLB, CBLC, CDKN2A, CEBPA, CREBBP, CSF3R, CUX1, DNMT3A, ETV6, EZH2, FLT3, GATA1, GATA2, GNAS, HRAS, IDH1, IDH2, IKZF1, JAK2, JAK3, KDM6A, KIT, KMT2A, KMT2D, KRAS, MPL, MYD88, NOTCH1, NPM1, NRAS, PDGFRA, PHF6, PTEN, PTPN11, RAD21, RUNX1, SETBP1, SF3B1, SMC1A, SMC3, STAG2, TET2, TP53, WT1, ZRSR2 Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| FISH for chromosome 4/10/17, ALL | Hemato-oncology | 5 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. Clinical indication and BMA diagnosis is must** | Bone marrow aspirate? | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate | FISH |
| FISH for JAK2 (9p24) gene rearrangement, MPN | Hemato-oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | FISH |
| FISH for FGFR1(8p11.2) gene rearrangement, MPN | Hemato-oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | FISH |
| FISH for t(14;20), IGH/MAFB,MM | Hemato-oncology | 7 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. Clinical indication and BMA diagnosis is must** | Bone marrow aspirate? | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate | FISH |
| FISH for t(6;9)(p22;q34), DEK/NUP, AML | Hemato-oncology | 5 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. Clinical indication and BMA diagnosis is must** | Bone marrow aspirate? | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate | FISH |
| FLT3-ITD mutant allele burden analysis | Hemato-oncology | 4 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone aspirate in EDTA; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Fragment analysis |
| JAK2 gene analysis - 2 exons (12, 14) by NGS | Hemato-oncology | 7 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| JAK2 gene analysis - Exon 14 | Hemato-oncology | 7 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Sanger sequencing |
| JMML risk stratification gene panel | Hemato-oncology | 14 working days | CBLC, KRAS, NRAS, HRAS, PTPN11, SETBP1, JAK3, CBL, ASXL1, RUNX1, TET2, JAK2, EZH2 Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| Leukemia/Lymphoma Panel- Flowcytometry | Hemato-oncology | 2 working days | Appropriately labelled air-dried and unstained Bone marrow aspirate smears and Peripheral blood smears must accompany every specimen. | Peripheral blood alongwith bone marrow aspirate in EDTA | Bone marrow smears on slides; bone marrow aspirate in EDTA; EDTA anticoagulated peripheral blood | 2-8℃ | Minimum of 2 bone marrow smears; minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral bloo | Flowcytometry |
| MDS prognostication and risk stratification gene panel | Hemato-oncology | 14 working days | ATRX, ASXL1, BCOR, CALR, CUX1, ETV6/TEL, EZH2, DNMT3A, GATA1, TET2, IDH1, TP53, NRAS/KRAS, RUNX1, SF3B1, ZRSR2, STAG2, SETBP1, IDH2 Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| MDS-AML Familial gene panel | Hemato-oncology | 14 working days | CEBPA,GATA2,RUNX Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| MPN - CALR (exon 9) gene analysis | Hemato-oncology | 7 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/purified genomic DNA/bone marrow aspirate | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; bone Marrow in EDTA | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Fragment analysis |
| MPN prognostication and risk stratification panel | Hemato-oncology | 14 working days | ASXL1, CALR, JAK2, MPL, DNMT3A, TET2 Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate/purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| Myelodysplasia Panel - Flowcytometry | Hemato-oncology | 2 working days | Provide detailed clinical history along with CBC reports[Note : Peripheral blood is not acceptable for this panel] | Peripheral blood along with bone marrow aspirate in EDTA | Bone marrow aspirate in EDTA | 2-8℃ | Minimum 1ml of bone marrow aspirate | Flowcytometry |
| Myeloproliferative Neoplasms panel(MPN), 4 markers- PDGFRA gene rearrangement, PDGFRB gene rearrangement, JAK2 gene rearrangement, FGFR1 gene rearrangement. FISH | Hemato-oncology | 6 working days | Includes PDGFRA , PDGFRB, FGFR1, JAK2 gene rearrangement | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | FISH |
| NPM1 gene analysis (Hot Spot - exon 12) | Hemato-oncology | 14 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/purified genomic DNA/bone marrow aspirate | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; bone marrow in EDTA | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Fragment analysis |
| PML-RARA gene fusion analysis (Qualitative) | Hemato-oncology | 2 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood/bone marrow aspirate | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA | Room temperature (refrigerate overnight if necessary) | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | RT-PCR |
| Agammaglobulinemia (BTK) gene analysis | Immunology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Chimerism testing | Immunology | 5 working days | 16 STR loci present on different chromosomes are evaluated from patients and donor before transplant and monitor the presence or absence in patient post transplant | Pre-transplant samples for patient and donor: peripheral blood/purified genomic DNA/buccal swabs Po | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; buccal swabs in a sterile tube w | 20-25℃ | Minimum 5ml peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); mi | Fragment Analysis |
| Congenital neutropenia gene panel | Immunology | 21 working days | CLPB, CSF3R, ELANE, G6PC3, GATA1, GFI1, HAX1, JAGN1, USB1, VPS45, WAS | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| CYP3A5 testing for Tacrolimus dosing | Immunology | 7 working days | Not Available | Peripheral blood in EDTA | EDTA anticoagulated peripheral blood | 20-25℃ | Minimum 3ml of peripheral blood | Sanger sequencing |
| HLA B27 testing | Immunology | 7 working days | Label each tube clearly with name/Age/Sex | Peripheral blood; purified genomic DNA; buccal swabs (4) for patients on chemotherapy or anemic patient | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; buccal swabs in a sterile container | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| HLA B51 testing | Immunology | 7 working days | Label each tube clearly with name/Age/Sex | Peripheral blood; purified genomic DNA; buccal swabs (4) for patients on chemotherapy or anemic pati | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; buccal swabs in a sterile contai | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| HLA Typing confirmation (High resolution) | Immunology | 5 working days | Label each tube clearly with name/Age/Sex | Peripheral blood; purified genomic DNA; buccal swabs (4) for patients on chemotherapy or anemic pati | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; buccal swabs in a sterile contai | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| HLA Typing High resolution (HLA A, B, C, DRB1, DQB1) | Immunology | 10 working days | Label each tube clearly with name/Age/Sex | Peripheral blood; purified genomic DNA; buccal swabs (4) for patients on chemotherapy or anemic patient | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; buccal swabs in a sterile container | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| HLA Typing High resolution (HLA A, B, C, DRB1, DQB1) - Expedited TAT | Immunology | 7 working days | Label each tube clearly with name/Age/Sex | Peripheral blood; purified genomic DNA; buccal swabs (4) for patients on chemotherapy or anemic patient | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; buccal swabs in a sterile container | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| HLA typing low resolution (HLA A, B, DRB1) | Immunology | 10 working days | Label each tube clearly with name/Age/Sex | Peripheral blood; purified genomic DNA; buccal swabs (4) for patients on chemotherapy or anemic patient | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; buccal swabs in a sterile container | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| HLA-B* 1502 for carbamazepine toxicity | Immunology | 10 working days | HLA-B* locus is evaluated to identify the HLA-B 1502 variation which is linked to Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) complications in patients receiving Carbamazepine | Peripheral blood; purified genomic DNA; buccal swabs (4) for patients on chemotherapy or anemic patient | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; buccal swabs in a sterile container | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hyper-immunoglobulin E syndrome (DOCK8) gene sequencing | Immunology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| IKBKG deletion/duplication analysis | Immunology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Lymphoproliferative Disorder Classifier Panel - Flowcytometry | Immunology | 2 working days | Appropriately labelled air-dried and unstained Bone marrow aspirate smears and Peripheral blood smears must accompany every specimen. | Peripheral blood along with bone marrow aspirate in EDTA. Peripheral blood can be accepted if blasts/ | Bone marrow smears on slides; bone marrow aspirate in EDTA; EDTA anticoagulated peripheral blood | 2-8℃ | Minimum of 2 bone marrow smears; minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | Flowcytometry |
| Primary immunodeficiency gene panel | Immunology | 21 working days | ACP5, ACTB, ADA, AGA, AICDA, AIRE, AK2, ALG13, AP3B1, AP4E1, APOL1, ATM, B2M, BLM, BLNK, BLOC1S3, BLOC1S6, BTK, C1QA, C1QB, C1QC, C1R, C1S, C2, C3, C4A, C4B, C5, C6, C7, C8A, C8B, C9, CARD11, CARD9, CASP10, CASP8, CD19, CD247, CD27, CD3D, CD3E, CD3G, CD40, CD40LG, CD46, CD55, CD59, CD79A, CD79B, CD81, CD8A, CEBPE, CFB, CFD, CFH, CFHR1, CFHR3, CFHR5, CFI, CFP, CHD7, CIITA, CLEC7A, COLEC11, CORO1A, CR2, CREBBP, CSF2RA, CSF3R, CTSC, CXCR4, CYBA, CYBB, DCLRE1C, DHFR, DKC1, DNMT3B, DOCK8, DTNBP1, ELANE, EPG5, ERCC2, ERCC3, F12, FADD, FAS, FASLG, FCGR1A, FCGR3A, FCN3, FERMT3, FOXN1, FOXP3, G6PC, G6PC3, G6PD, GATA2, GFI1, GJC2, GTF2H5, HAX1, HPS1, HPS3, HPS4, HPS5, HPS6, ICOS, IFNGR1, IFNGR2, IGHG2, IGHM, IGKC, IGLL1, IKZF1, IL10, IL10RA, IL10RB, IL12B, IL12RB1, IL17F, IL17RA, IL1RN, IL2, IL21, IL21R, IL2RA, IL2RG, IL36RN, IL7R, INSR, IRAK4, IRF8, ITCH, ITGB2, ITK, JAK2, JAK3, KMT2D, KRAS, LAMTOR2, LCK, LIG1, LIG4, LPIN2, LRBA, LRRC8A, LYST, MAGT1, MALT1, MAN2B1, MANBA, MASP1, MASP2, MBL2, MC2R, MCM4, MEFV, MLPH, MPO, MRE11A, MS4A1, MSH6, MTHFD1, MVK, MYD88, MYO5A, NBN, NCF1, NCF2, NCF4, NCSTN, NFKB1, NFKB2, NFKBIA, NHEJ1, NHP2, NKX2- 5, NLRP12, NLRP3, NOD2, NOP10, NRAS, ORAI1, PCCA, PCCB, PEPD, PGM3, PIGA, PIK3CD, PIK3R1, PLCG2, PLG, PMM2, PMS2, PNP, PRF1, PRKCD, PRKDC, PRPS1, PSENEN, PSMB8, PSTPIP1, PTPN11, PTPRC, PTRF, RAB27A, RAC2, RAG1, RAG2, RASGRP2, RBCK1, RECQL4, RFX5, RFXANK, RFXAP, RNASEH2A, RNASEH2B, RNASEH2C, RNF168, RORC, RPSA, RTEL1, SAMHD1, SBDS, SERAC1, SERPING1, SH2D1A, SKIV2L, SLC35A1, SLC35C1, SLC37A4, SLC39A4, SLC46A1, SMARCAL1, SP110, SPINK5, STAT1, STAT2, STAT3, STAT4, STAT5B, STIM1, STK4, STX11, STXBP2, TAP1, TAP2, TAPBP, TAZ, TBX1, TCIRG1, TCN2, TERT, TFRC, THBD, TICAM1, TINF2, TLR3, TMC6, TMC8, TNFRSF11A, TNFRSF13B, TNFRSF13C, TNFRSF1A, TNFRSF4, TRAC, TRAF3, TREX1, TTC37, TYK2, UNC119, UNC13D, UNC93B1, UNG, USB1, VPS13B, VPS45, WAS, WIPF1, WRAP53, XIAP, ZAP70, ZBTB24 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Severe combined immunodeficiency (SCID) gene panel | Immunology | 21 working days | ADA, AK2, CD3D, CD3E, CIITA, DCLRE1C, IL2, IL21R, IL2RG, IL7R, JAK3, NHEJ1, PNP, PTPRC, RAG1, RAG2, RFX5, RFXANK, RFXAP, TAP1, TAPBP | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Thrombotic Thrombocytopenic Purpura (ADAMTS13) gene analysis | Immunology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| TPMT and NUDT15 gene analysis | Immunology | 10 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Sanger Sequencing |
| Alpha-mannosidosis (MAN2B1) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Biotinidase deficiency (BTD) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Citrullinemia gene panel | Metabolic disorders | 21 working days | ASS1, SLC25A13, SLC25A15 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Fabry disease (GLA) deletion/duplication analysis | Metabolic disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Fabry disease (GLA) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Fanconi bickel syndrome (SLC2A2) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Farber lipogranulomatosis (ASAH1) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Fatty acid oxidation disorders gene panel | Metabolic disorders | 21 working days | ACAD9, ACADL, ACADM, ACADS, ACADSB, ACADVL, CPT1A, CPT1B, CPT2, ETFA, ETFB, ETFDH, GLUD1, HADH, HADHA, HADHB, HMGCL, HMGCS2, HSD17B10, LPIN1, MLYCD, SLC22A5, SLC25A20, TAZ | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Fucosidosis (FUCA1) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Galactosemia (GALT) gene analysis | Metabolic Disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Galactosialidosis (CTSA) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| GBA gene sequencing | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| GLUT1 deficiency (SLC2A1) deletion/duplication analysis | Metabolic disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| GLUT1 deficiency (SLC2A1) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Glycine encephalopathy (GLDC) deletion/duplication analysis | Metabolic disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Glycine encephalopathy gene panel | Metabolic disorders | 21 working days | AMT, GCSH, GLDC | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Glycogen storage disorder gene panel | Metabolic disorders | 21 working days | AGL, ALDOA, ENO3, G6PC, GAA, GBE1, GYG1, GYS1, GYS2, LAMP2, LDHA, PFKM, PGAM2, PGM1, PHKA1, PHKA2, PHKB, PHKG2, PRKAG2, PYGL, PYGM, SLC2A2, SLC37A4 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Glycosylation (CDG) disorders gene panel | Metabolic disorders | 21 working days | ALG1, ALG11, ALG12, ALG13, ALG14, ALG2, ALG3, ALG6, ALG8, ALG9, ATP6V0A2, B3GLCT, B3GAT3, B4GALT1, B4GALT7, CAD, CCDC115, CHST14, CHST3, CHST6, CHSY1, COG1, COG4, COG5, COG6, COG7, COG8, DDOST, DHDDS, DOLK, DPAGT1, DPM1, DPM2, DPM3, EXT1, EXT2, FKRP, FKTN, GALNT3, GFPT1, GNE, LARGE, LFNG, MAN1B1, MGAT2, MOGS, MPDU1, MPI, NGLY1, PGM1, PIGA, PIGL, PIGM, PIGO, PIGV, PMM2, POMGNT1, POMT1, POMT2, RFT1, SEC23B, SLC35A1, SLC35A2, SLC35C1, SLC35D1, SRD5A3, SSR4, ST3GAL3, ST3GAL5, STT3A, STT3B, TMEM165, TUSC3 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| GM1 gangliosidosis/mucopolysaccharidosis type IVB (GLB1) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hereditary fructose intolerance (ALDOB) gene sequencing | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Homocystinuria gene panel | Metabolic disorders | 21 working days | ABCD4, CBS, HCFC1, LMBRD1, MMACHC, MMADHC, MTHFR, MTR, MTRR | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hyperargininemia (ARG1) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Leigh syndrome & mitochondrial encephalopathy gene panel | Metabolic disorders | 21 working days | AARS, AARS2, ABCB11, ABCB4, ABCB7, ABCD4, ACAD9, ACADM, ACADVL, ACO2, ACSF3, ADCK3, ADCK4, AFG3L2, AGK, AGL, AIFM1, ALAS2, ALDOA, ALDOB, ALG1, ALG11, ALG13, ALG2, ALG3, ALG6, ALG9, AMACR, APOPT1, APTX, ARG1, ASL, ASS1, ATP5A1, ATP5E, ATP7B, ATP8B1, ATPAF2, AUH, B4GALT1, BCKDHA, BCKDHB, BCS1L, BOLA3, C10ORF2, C12ORF65, C19ORF12, CA5A, CARS2, CHKB, CISD2, CLPB, COA5, COA6, COASY, COG4, COG5, COG6, COG7, COG8, COQ2, COQ4, COQ6, COQ9, COX10, COX14, COX15, COX20, COX4I2, COX6A1, COX6B1, COX7B, CPS1, CPT1A, CPT2, CYC1, DARS, DARS2, DBT, DDHD1, DDHD2, DDOST, DGUOK, DLAT, DLD, DMGDH, DNA2, DNAJC19, DNM1L, DNM2, DOLK, DPAGT1, DPM1, DPM3, EARS2, ECHS1, ELAC2, ENO3, ETFA, ETFB, ETFDH, ETHE1, FAH, FARS2, FASTKD2, FBP1, FBXL4, FDX1L, FH, FLAD1, FOXRED1, G6PC, GAA, GAMT, GARS, GATM, GBE1, GCDH, GFER, GFM1, GFM2, GLRX5, GMPPA, GSS, GTPBP3, GYG1, GYG2, GYS1, GYS2, HADHA, HADHB, HARS2, HCFC1, HIBCH, HLCS, HMGCL, HMGCS2, HSD17B10, HSPD1, IARS2, IBA57, ISCA2, ISCU, IVD, LAMP2, LARS, LARS2, LDHA, LIAS, LIPT1, LMBRD1, LRPPRC, LYRM4, LYRM7, MARS, MARS2, MCCC1, MCCC2, MCEE, MFF, MFN2, MGAT2, MGME1, MICU1, MLYCD, MMAA, MMAB, MMACHC, MMADHC, MOGS, MPC1, MPDU1, MPI, MPV17, MRPL12, MRPL3, MRPL44, MRPS16, MRPS22, MRPS7, MTFMT, MTO1, MTPAP, MTR, MTRR, MUT, NADK2, NAGS, NARS2, NDUFA1, NDUFA10, NDUFA11, NDUFA12, NDUFA13, NDUFA2, NDUFA4, NDUFA9, NDUFAF1, NDUFAF2, NDUFAF3, NDUFAF4, NDUFAF5, NDUFAF6, NDUFAF7, NDUFB3, NDUFB9, NDUFS1, NDUFS2, NDUFS3, NDUFS4, NDUFS6, NDUFS7, NDUFS8, NDUFV1, NDUFV2, NFS1, NFU1, NGLY1, NR2F1, NUBPL, OPA1, OPA3, OTC, PARS2, PC, PCCA, PCCB, PDHA1, PDHB, PDHX, PDP1, PDSS1, PDSS2, PET100, PFKM, PGAM2, PGM1, PHKA1, PHKA2, PHKB, PHKG2, PMM2, PNPT1, POLG, POLG2, PRKAG2, PRPS1, PTRH2, PUS1, PYGM, QARS, RANBP2, RARS, RARS2, REEP1, RFT1, RMND1, RRM2B, SARS2, SCO1, SCO2, SDHA, SDHAF1, SERAC1, SFXN4, SLC19A2, SLC19A3, SLC22A5, SLC25A1, SLC25A13, SLC25A15, SLC25A19, SLC25A20, SLC25A22, SLC25A3, SLC25A38, SLC25A4, SLC2A2, SLC35A1, SLC35A2, SLC35C1, SLC37A4, SLC6A8, SLC7A7, SPAST, SPG7 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Lysosomal acid lipase deficiency (LIPA) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Maple syrup urine disease gene panel | Metabolic disorders | 21 working days | BCKDHA, BCKDHB, DBT, DLD, PPM1K | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| McArdle disease (PYGM) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Menkes disease (ATP7A) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Methylmalonic aciduria gene panel | Metabolic disorders | 21 working days | ABCD4, ACSF3, CD320, HCFC1, LMBRD1, MCEE, MMAA, MMAB, MMACHC, MMADHC, MUT, SUCLA2, SUCLG1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Mucopolysaccharidosis gene panel | Metabolic disorders | 21 working days | ARSB, GALNS, GLB1, GNS, GUSB, HGSNAT, HYAL1, IDS, IDUA, NAGLU, SGSH, SUMF1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Niemann-Pick disease gene panel | Metabolic disorders | 21 working days | NPC1, NPC2, SMPD1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Organic acidemia gene panel | Metabolic disorders | 21 working days | ABCD4, ACAT1, ACAT2, ACSF3, ALDH5A1, ASL, ASPA, AUH, BCKDHA, BCKDHB, BTD, CblC, CD320, CLPB, D2HGDH, DBT, DHTKD1, DLD, DLST, DNAJC19, ETFA, ETFB, ETFDH, ETHE1, FH, GCDH, GLYCTK, HCFC1, HLCS, HMGCL, HMGCS2, HSD17B10, IDH2, IVD, L2HGDH, LMBRD1, MCCC1, MCCC2, MCEE, MLYCD, MMAA, MMAB, MMACHC, MMADHC, MUT, MVK, OGDH, OPA3, OXCT1, PCCA, PCCB, SERAC1, SLC25A1, SUCLA2, SUCLG1, SUGCT, TAZ, UMPS | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Ornithine transcarbamylase deficiency (OTC) deletion/duplication analysis | Metabolic disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Phenylketonuria (PAH) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Pompe disease (GAA) deletion/duplication analysis | Metabolic disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Pompe disease (GAA) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Sialidosis (NEU1) gene analysis | Metabolic disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Urea cycle defects gene panel | Metabolic disorders | 21 working days | ARG1, ASL, ASS1, CPS1, NAGS, OTC, SLC25A13, SLC25A15 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Alport syndrome gene panel | Nephrology | 21 working days | COL4A3,COL4A4,COL4A5 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hemolytic uremic syndrome (CFH, CFHR1 & CFHR3) deletion duplication analysis | Nephrology | 14 working days | Provide detailed clinical history along with Renal biopsy report | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Meckel Gruber syndrome gene panel | Nephrology | 21 working days | B9D1, B9D2, CC2D2A, CEP290, KIF14, MKS1, NPHP3, RPGRIP1L, TCTN2, TMEM216, TMEM231, TMEM67 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Nephrotic syndrome gene panel | Nephrology | 21 working days | ACTN4, ADCK4, ALG1, ALMS1, ANLN, APOL1, ARHGAP24, ARHGDIA, CD151, CD2AP, CFH, COL4A3, COL4A4, COL4A5, COQ2, COQ6, COQ7, COQ9, CRB2, CUBN, DGKE, EMP2, EXT1, FAT1, GATA3, INF2, ITGA3, ITGB4, KANK1, KANK2, KANK4, KIAA2022, LAMB2, LMNA, LMX1B, MAFB, MAGI2, MEFV, MYH9, MYO1E, NEIL1, NEU1, NPHS1, NPHS2, NUP107, NUP205, NUP93, NXF5, PAX2, PDSS2, PLCE1, PMM2, PTPRO, SCARB2, SMARCAL1, TRPC6, TTC21B, WDR73, WT1, XPO5, ZMPSTE24 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Polycystic kidney disease gene panel | Nephrology | 21 working days | GANAB, MUC1, PKD1, PKD2, PKHD1, UMOD | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Primary hyperoxaluria gene panel | Nephrology | 21 working days | AGXT, GRHPR, HOGA1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Xanthinuria gene panel | Nephrology | 21 working days | MOCOS, XDH | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Ataxia Telengiectasia(chromosome instability syndrome) | Neurology | 15 working days | Not Available | Peripheral Blood | Sodium heparin-Green top | 20-25℃ | Minimum 4 ml peripheral blood | Cytogenetics/Karyotyping |
| ATRX gene analysis | Neurology | 21 working days | For genetic analysis of Alpha thalassemia X-linked intellectual disability syndrome &/or alpha thalassemia myelodysplastic syndrome (ATMDS). [Note : Thalassemia screening/MDS flow cytometry report should be attached ] | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Brown Vialetto-Van Laere syndrome gene panel | Neurology | 21 working days | ?SLC52A2 & SLC52A3 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Comprehensive neurology panel | Neurology | 21 working days | Comprehensive Neurology Panel Genes (1475 genes) are listed in the APPENDIX | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| DCX & PAFAH1B1 deletion/duplication analysis | Neurology | 14 working days | DCX & PAFAH1B1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Familial hemiplegic migraine gene panel | Neurology | 21 working days | ATP1A2, CACNA1A, PRRT2, SCN1A | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Fragile X Syndrome | Neurology | 15 working days | Not Available | Peripheral Blood | Sodium heparin-Green top | 20-25℃ | Minimum 4 ml peripheral blood | Cytogenetics/Karyotyping |
| Lissencephaly gene panel | Neurology | 21 working days | ACTB, ACTG1, ADGRG1, ARX, ATP6V0A2, B3GALNT2, B4GAT1, CDK5, DCX, DYNC1H1, FKRP, FKTN, FTO, ISPD, KATNB1, KIAA1279, KIF2A, KIF5C, LAMA2, LAMB1, LAMC3, LARGE, NDE1, OCLN, PAFAH1B1, PHGDH, POMGNT1, POMGNT2, POMK, POMT1, POMT2, RAB18, RAB3GAP1, RAB3GAP2, RELN, RTTN, SNAP29, SRD5A3, TBC1D20, TMEM5, TMTC3, TUBA1A, TUBA8, TUBB, TUBB2A, TUBB2B, TUBB3, TUBB4A, TUBG1, VIPAS39, VLDLR, VPS33B, WDR62 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| MECP2 gene sequencing | Neurology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Microcephaly gene panel | Neurology | 21 working days | ANKLE2, ARFGEF2, ASPM, ASXL3, ATR, ATRX, CASC5, CASK, CDC6, CDK5RAP2, CDK6, CDKL5, CDT1, CENPE, CENPJ, CEP135, CEP152, CEP63, CIT, CRIPT, DIAPH1, DYRK1A, FOXG1, IER3IP1, KATNB1, KIF11, LIG4, MCPH1, MECP2, MED17, MFSD2A, MSMO1, NBN, NDE1, NHEJ1, NIN, ORC1, ORC4, ORC6, PCNT, PHC1, PLK4, PNKP, PPP1R15B, QARS, RAB18, RAB3GAP1, RAB3GAP2, RAD50, RBBP8, RTTN, SASS6, SLC25A19, SLC2A1, SLC9A6, STAMBP, STIL, TBC1D20, TCF4, TRAPPC9, TRMT10A, TSEN2, TSEN34, TSEN54, TUBGCP4, TUBGCP6, UBE3A, WDFY3, WDR62, XRCC4, ZEB2, ZNF335 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Neuronal migration disorder gene panel | Neurology | 21 working days | ACTB, ACTG1, ADGRG1, AKT3, ARFGEF2, ARX, B3GALNT2, B4GAT1, CCND2, CDK5, COL4A1, COL4A2, DCX, DEPDC5, DYNC1H1, EMX2, ERMARD, FAT4, FIG4, FKRP, FKTN, FLNA, GMPPB, ISPD, KATNB1, KIAA1279, KIF2A, KIF5C, L1CAM, LAMB1, LARGE, MCPH1, NDE1, NEDD4L, OCLN, PAFAH1B1, PI4KA, PIK3CA, PIK3R2, POMGNT1, POMGNT2, POMK, POMT1, POMT2, RELN, RTTN, SHH, SIX3, SRPX2, TMEM5, TUBA1A, TUBA8, TUBB, TUBB2A, TUBB2B, TUBB3, TUBG1, WDR62 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Pontocerebellar hypoplasia gene panel | Neurology | 21 working days | AMPD2, CASK, CHMP1A, CLP1, EXOSC3, EXOSC8, PCLO, RARS2, SEPSECS, TBC1D23, TOE1, TSEN15, TSEN2, TSEN34, TSEN54, VPS53, VRK1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Rett Syndrome (MECP2) deletion/duplication analysis | Neurology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Rett Syndrome gene panel | Neurology | 21 working days | CDKL5, FOXG1, MECP2, MEF2C | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Aicardi-Goutieres syndrome gene panel | Neurology - Epilepsy | 21 working days | ADAR, IFIH1, RNASEH2A, RNASEH2B, RNASEH2C, SAMHD1, TREX1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Benign infantile epilepsy gene panel | Neurology - Epilepsy | 21 working days | KCNQ2, KCNQ3, PRRT2, SCN2A, SCN8A | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Dravet syndrome (SCN1A) deletion/duplication analysis | Neurology - Epilepsy | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Dravet syndrome (SCN1A) gene analysis | Neurology - Epilepsy | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Early infantile epileptic encephalopathy-4 (STXBP1) deletion/duplication analysis | Neurology - Epilepsy | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Epileptic encephalopathy gene panel | Neurology - Epilepsy | 21 working days | AARS, ABAT, ABCC8, ALDH7A1, ALG13, AMT, AP3B2, ARHGEF9, ARV1, ARX, ATP13A2, ATP7A, CACNA1A, CACNA1H, CACNB4, CAD, CDKL5, CHD2, CHRNA2, CHRNA4, CHRNB2, CLCN2, CLN3, CLN5, CLN6, CLN8, CLTC, CTSD, CTSF, D2HGDH, DENND5A, DHDDS, DNAJC5, DNM1, DOCK7, EEF1A2, FGF12, FOXG1, FRRS1L, GABBR2, GABRA1, GABRB2, GABRB3, GABRD, GABRG2, GAMT, GLDC, GNAO1, GRIN2B, GRIN2D, GRN, GUF1, HCN1, HNRNPU, HSD17B4, IDH2, ITPA, KCNA2, KCNB1, KCNJ11, KCNQ2, KCNQ3, KCNT1, KCTD7, MBD5, MDH2, MECP2, MFSD8, NECAP1, NTRK2, NUS1, PC, PCDH19, PEX1, PEX10, PEX12, PEX26, PEX6, PIGA, PLCB1, PNKP, PNPO, PPT1, SCN1A, SCN1B, SCN2A, SCN8A, SCN9A, SIK1, SLC12A5, SLC13A5, SLC1A2, SLC25A22, SLC2A1, SLC35A2, SNAP25, SPTAN1, ST3GAL3, STXBP1, SUOX, SYNJ1, SZT2, TBC1D24, TCF4, TPP1, TSC1, TSC2, UBA5, UBE3A, WWOX, ZEB2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Familial female mental retardation/epilepsy gene panel | Neurology - Epilepsy | 21 working days | ALDH7A1, ARX, ATRX, CASK, CDKL5, CUL4B, FOLR1, GRIA3, HSD17B10, IQSEC2, KCNQ2, KCNQ3, KDM5C, MECP2, MED12, MEF2C, OPHN1, PCDH19, PGK1, PHF6, PNPO, POLG, SCN1A, SCN1B, SCN2A, SCN8A, SLC2A1, SLC9A6, SPTAN1, STXBP1, UBE2A | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Progressive myoclonic epilepsy gene panel | Neurology - Epilepsy | 21 working days | ADRA2B, ASAH1, ATP13A2, CERS1, CLN3, CLN5, CLN6, CLN8, CSTB, CTSD, CTSF, DNAJC5, EPM2A, FOLR1, GOSR2, GRN, KCNC1, KCTD7, LMNB2, MFSD8, NEU1, NHLRC1, PPT1, PRDM8, PRICKLE1, PRICKLE2, SCARB2, TPP1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| TBC1D24 gene analysis | Neurology - Epilepsy | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Ataxia-telangiectasia (ATM) deletion/duplication analysis | Neurology - Movement Disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Ataxia-telangiectasia (ATM) gene analysis | Neurology - Movement Disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Dystonia gene panel | Neurology - Movement Disorders | 21 working days | ACTB, AFG3L2, ANO3, ARSA, ATM, ATP1A3, ATP6AP2, ATP7B, AUH, BCAP31, C19orf12, CACNA1A, CACNA1B, CACNA1G, CCDC88C, CIZ1, COASY, COL6A3, DDC, DNAJC13, DNAJC6, DRD2, EEF2, ELOVL4, ELOVL5, FBXO7, FGF14, FTL, GBA, GCDH, GCH1, GNAL, HEXA, HPCA, HTRA2, ITPR1, KCNC3, KCND3, KCNMA1, KCTD17, KMT2B, LRRK2, MAPT, MECP2, MR1, NKX2-1, NPC1, NPC2, PANK2, PARK2, PARK7, PDYN, PINK1, PLA2G6, PNKD, PPP2R2B, PRKAG2, PRKCG, PRKRA, PRRT2, SGCE, SLC2A1, SLC30A10, SLC6A3, SMPD1, SNCA, SPR, SPTBN2, SYNJ1, TAF1, TGM6, TH, THAP1, TIMM8A, TMEM240, TOR1A, TRPC3, TTBK2, TUBB4A, UCHL1, VPS13A, VPS35, WDR45 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Early-onset juvenile parkinsonism gene panel | Neurology - Movement Disorders | 21 working days | ATP13A2, DNAJC6, FBXO7, LRRK2, PARK2, PARK7, PINK1, PLA2G6, RAB39B, SLC6A3, SNCA, SYNJ1, VPS13C | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Episodic ataxia gene panel | Neurology - Movement Disorders | 21 working days | CACNA1A, CACNB4, KCNA1, SLC1A3 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hyperekplexia gene panel | Neurology - Movement Disorders | 21 working days | ARHGEF9, GLRA1, GLRB, SLC6A5 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Neurotransmitter disorders gene panel | Neurology - Movement Disorders | 21 working days | ABAT, ALDH5A1, ALDH7A1, AMT, ARHGEF9, ATP13A2, C19orf12, CACNA1A, CACNA1S, CACNB2, CACNB4, COASY, DBH, DDC, DNAJC6, FBXO7, FTL, GAD1, GCH1, GCSH, GLDC, GLRA1, GLRB, GPHN, KCNA1, LRRK2, MAOA, MAOB, PANK2, PARK2, PARK7, PCBD1, PHGDH, PINK1, PLA2G6, PNPO, PSAT1, PSPH, PTS, QDPR, RAB39B, SCN4A, SLC18A2, SLC1A3, SLC25A22, SLC6A3, SLC6A5, SNCA, SPR, SYNJ1, TH, VPS13C, WDR45 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| X-linked spastic paraplegia-2 (PLP1) deletion/duplication analysis | Neurology - Movement Disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Neurofibromatosis (NF1 and NF2) gene analysis | Neurology - neurocutaneous | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Neurofibromatosis type 1 (NF1) deletion/duplication analysis | Neurology - neurocutaneous | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Neurofibromatosis type 2 (NF2) deletion/duplication analysis | Neurology - neurocutaneous | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Neurofibromatosis type 2 (NF2) gene analysis | Neurology - neurocutaneous | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| TSC1 & TSC2 gene analysis | Neurology - neurocutaneous | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| TSC1 deletion/duplication analysis | Neurology - neurocutaneous | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| TSC2 deletion/duplication analysis | Neurology - neurocutaneous | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| 4H syndrome gene panel | Neurology - neurodegenerative | 21 working days | POLR3A, POLR3B | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Adrenoleukodystrophy (ABCD1) gene analysis | Neurology - neurodegenerative | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Alkaptonuria (HGD) gene analysis | Neurology - neurodegenerative | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Canavan disease (ASPA) gene analysis | Neurology - neurodegenerative | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Cystic megalencephaly (MLC1) deletion/duplication analysis | Neurology - neurodegenerative | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Cystic megalencephaly (MLC1) gene analysis | Neurology - neurodegenerative | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Giant axonal neuropathy-1 (GAN) gene analysis | Neurology - neurodegenerative | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hypomyelination syndrome gene panel | Neurology - neurodegenerative | 21 working days | AIMP1, BCAP31, C11ORF73, DARS, EGR2, EIF2B1, EIF2B2, EIF2B3, EIF2B4, EIF2B5, ERCC4, ERCC5, ERCC6, ERCC8, EXOSC8, FAM126A, GJC2, HSPD1, MLC1, MPZ, PLP1, POLR1C, POLR3A, POLR3B, PYCR2, RARS, SLC25A12, SLC33A1, SPTAN1, STXBP1, TBCD, TUBB4A, VPS11 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Joubert syndrome gene panel | Neurology - neurodegenerative | 21 working days | AHI1, ARL13B, B9D1, C2CD3, C5orf42, CC2D2A, CEP104, CEP290, CEP41, CSPP1, DDX59, INPP5E, KIAA0556, KIAA0586, KIAA0753, KIF7, LAMA1, MKS1, NPHP1, OFD1, PDE6D, RPGRIP1L, TCTN1, TCTN2, TCTN3, TMEM138, TMEM216, TMEM231, TMEM237, TMEM67, TTC21B, ZNF423 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Krabbe disease (GALC) deletion/duplication analysis | Neurology - neurodegenerative | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Krabbe disease (GALC) gene analysis | Neurology - neurodegenerative | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Leukodystrophy gene panel | Neurology - neurodegenerative | 21 working days | AARS, AARS2, ABCD1, ABCD4, ACAD9, AARS, AARS2, ABCD1, ABCD4, ACAD9, ACOX1, ACP5, ACSF3, ADAR, ADGRG1, ADSL, AGA, AGK, AIMP1, ALDH3A2, ALDH5A1, ALG1, ALG11, ALG12, ALG13, ALG2, ALG3, ALG6, ALG8, ALG9, AMT, ANO5, AP3B1, ARSA, ARSB, ASPA, ATP13A2, ATP6V0A2, ATP7A, B3GALNT2, B4GALT1, B4GAT1, BCAP31, BCKDHA, BCKDHB, BLOC1S6, BTD, C10orf2, CAD, CAPN3, CARS2, CAV3, CBS, CD27, CD320, CHKB, CLCN2, CLN3, CLN5, CLN6, CLN8, COG1, COG4, COG5, COG6, COG7, COG8, COL12A1, COL4A1, COL4A2, COL6A1, COL6A2, COL6A3, CSF1R, CTC1, CTSD, CTSF, CYP27A1, D2HGDH, DAG1, DARS, DARS2, DBT, DCAF17, DCAF8, DDC, DDOST, DES, DGUOK, DLAT, DLD, DMD, DNAJB6, DNAJC5, DOLK, DPAGT1, DPM1, DPM2, DPM3, DYSF, EARS2, EIF2B1, EIF2B2, EIF2B3, EIF2B4, EIF2B5, EMD, ERCC2, ERCC3, ERCC4, ERCC5, ERCC6, ERCC8, ETFA, ETFB, ETFDH, FA2H, FAM126A, FARS2, FBXL4, FH, FHL1, FKRP, FKTN, FOLR1, FOXRED1, FUCA1, GALC, GALNS, GALT, GAN, GARS, GBE1, GCDH, GCSH, GFAP, GJA1, GJB1, GJC2, GLA, GLB1, GLDC, GM2A, GMPPB, GNPTAB, GNPTG, GNS, GPHN, GRN, GTF2H5, GUSB, HARS, HARS2, HCFC1, HEPACAM, HEXA, HGSNAT, HLCS, HMGCL, HNRNPDL, HSD17B4, HSPD1, HTRA1, HYAL1, IARS2, IDH2, IDS, IDUA, IFIH1, ISPD, ITGA7, ITK, IVD, JAM3, KARS, KCTD7, L2HGDH, LAMA2, LARGE, LARS, LARS2, LIAS, LMBRD1, LMNA, LMNB1, LYST, MAN2B1, MANBA, MARS, MARS2, MCCC1, MCCC2, MCEE, MCOLN1, MFSD8, MGAT2, MGME1, MLC1, MLYCD, MMAA, MMAB, MMACHC, MMADHC, MOCS1, MOCS2, MOGS, MPDU1, MPI, MPLKIP, MPV17, MTHFR, MTR, MTRR, MUT, MYOT, NAGLU, NARS2, NDUFA1, NDUFA11, NDUFA12, NDUFA2, NDUFA9, NDUFAF1, NDUFAF2, NDUFAF3, NDUFAF4, NDUFAF5, NDUFAF6, NDUFB3, NDUFB9, NDUFS1, NDUFS2, NDUFS3, NDUFS4, NDUFS6, NDUFS8, NDUFV1, NDUFV2, NEU1, NOTCH3, NPC1, NPC2, NUBPL, OCLN, OCRL, OPA1, PABPN1, PAH, PC, PCCA, PCCB, PDHA1, PDHB, PDHX, PDK3, PDP1, PDX1, PEX1, PEX10, PEX11B, PEX12, PEX13, PEX14, PEX16, PEX19, PEX2, PEX26, PEX3, PEX5, PEX6, PEX7, PGM1, PHGDH, PHYH, PLEC, PLP1, PMM2, POLG, POLR1C, POLR3A, POLR3B, POMGNT1, POMGNT2, POMK, POMT1, POMT2, PPT1, PRF1, PRPS1, PSAP, PYCR2, QARS, QDPR, RAB27A, RAR | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Metachromatic leukodystrophy gene panel | Neurology - neurodegenerative | 21 working days | ARSA, PSAP | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Neurodegeneration with brain iron accumulation 2B (PLA2G6) deletion/duplication analysis | Neurology - neurodegenerative | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Neurodegeneration with brain iron accumulation gene panel | Neurology - neurodegenerative | 21 working days | ATP13A2, COASY, C19orf12, CP, DCAF17, FA2H, FTL, PANK2, PLA2G6, WDR45 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Neuronal ceroid lipofuscinosis gene panel | Neurology - neurodegenerative | 21 working days | ATP13A2, CLN3, CLN5, CLN6, CLN8, CTSD, CTSF, DNAJC5, GRN, KCTD7, MFSD8, PPT1, TPP1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| NOTCH3 (CADASIL) gene analysis | Neurology - neurodegenerative | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Pantothenate kinase-associated neurodegeneration (PANK2) deletion/duplication analysis | Neurology - neurodegenerative | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Tay-Sachs disease (HEXA) deletion/duplication analysis | Neurology - neurodegenerative | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Tay-Sachs disease (HEXA) gene analysis | Neurology - neurodegenerative | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| X-linked adrenoleukodystrophy (ABCD1) deletion/duplication analysis | Neurology - neurodegenerative | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Arthrogryposis & congenital myasthenic syndrome gene panel | Neurology - neuromuscular | 21 working days | ADCY6, ADGRG6, AGRN, ALG14, ALG2, CHAT, CHRNA1, CHRNB1, CHRND, CHRNE, CHRNG, CHST14, CNTNAP1, COL13A1, COLQ, DNM2, DOK7, DPAGT1, ECEL1, ERBB3, FBN2, GFPT1, GLE1, LAMB2, LRP4, MUSK, MYBPC1, MYH3, MYH8, NALCN, PI4KA, PIEZO2, PIP5K1C, RAPSN, SCN4A, SLC18A3, SLC35A3, SNAP25, SYT2, TNNI2, TNNT3, TPM2, UBA1, VIPAS39, VPS33B, ZBTB42 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Calpainopathy/LGMD2A (CAPN3) deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Charcot-Marie-Tooth 1A/HNPP (PMP22, COX10, TEKT3) deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Charcot-Marie-Tooth and sensory neuropathies gene panel | Neurology - neuromuscular | 21 working days | AARS, AIFM1, ATL1, ATL3, CCT5, COX6A1, CTDP1, DHTKD1, DNAJB2, DNM2, DNMT1, DST, DYNC1H1, EGR2, FAM134B, FGD4, FIG4, GAN, GARS, GDAP1, GJB1, GNB4, HARS, HINT1, HK1, HOXD10, HSPB1, HSPB8, IGHMBP2, INF2, JPH1, KARS, KIF1A, KIF1B, KIF5A, LITAF, LMNA, LRSAM1, MARS, MED25, MFN2, MME, MORC2, MPZ, MTMR2, NAGLU, NDRG1, NEFH, NEFL, NGF, NTRK1, PDK3, PLEKHG5, PMP22, PRDM12, PRPS1, PRX, RAB7A, SBF1, SBF2, SCN11A, SCN9A, SH3TC2, SLC12A6, SLC25A46, SOX10, SPG11, SPTLC1, SPTLC2, SURF1, TFG, TRIM2, TRPV4, VCP, WNK1, YARS | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Charcot-Marie-Tooth type 4 (EGR2, GDAP1, NEFL, PRX) deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Congenital Muscular Dystrophy (LAMA2) deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Duchenne Muscular Dystrophy (DMD) deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Duchenne Muscular Dystrophy (DMD) gene sequencing | Neurology - neuromuscular | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Dysferlinopathy/LGMD2B (DYSF) deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Fukuyama Congenital Muscular Dystrophy (FKTN) gene sequencing (does not include repeat expansions) | Neurology - neuromuscular | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Fukuyama Congenital Muscular Dystrophy (FKTN) gene sequencing (does not include repeat expansions)[E | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Limb-girdle muscular dystrophy (SGCA, SGCB,SGCD, SGCG & FKRP) deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Muscular dystrophy & congenital myopathy gene panel | Neurology - neuromuscular | 21 working days | ACTA1, ANO5, B3GALNT2, B4GAT1, BAG3, BIN1, BVES, CAPN3, CAV3, CCDC78, CFL2, CHKB, CNTN1, COL12A1, COL6A1, COL6A2, COL6A3, CRYAB, DAG1, DES, DMD, DNAJB6, DNM2, DYSF, EMD, FHL1, FKRP, FKTN, FLNC, GMPPB, GNE, HNRNPA2B1, HNRNPDL, ISCU, ISPD, ITGA7, KBTBD13, KLHL40, KLHL41, LAMA2, LAMP2, LARGE, LDB3, LIMS2, LMNA, LMOD3, MEGF10, MTM1, MYF6, MYH2, MYH7, MYOT, NEB, PABPN1, PLEC, POGLUT1, POMGNT1, POMGNT2, POMK, POMT1, POMT2, RYR1, SEPN1, SGCA, SGCB, SGCD, SGCG, SMCHD1, SPEG, SYNE1, SYNE2, TCAP, TMEM43, TMEM5, TNNT1, TNPO3, TOR1AIP1, TPM2, TPM3, TRAPPC11, TRIM32, TTN, VCP | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Myotonia congenita (CLCN1) deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| PMP22 deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| PMP22 gene analysis (inflammatory demyelinating polyneuropathy screen) | Neurology - neuromuscular | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| POMT1 deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Spinal Muscular Atrophy (SMN1) gene analysis | Neurology - neuromuscular | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Sanger sequencing |
| Spinal Muscular Atrophy (SMN1/SMN2) deletion/duplication analysis | Neurology - neuromuscular | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Spinal Muscular Atrophy gene Panel | Neurology - neuromuscular | 21 working days | ASAH1, ASCC1, ATP7A, BICD2, BSCL2, CHCHD10, DNAJB2, DYNC1H1, FBXO38, GARS, HSPB8, IGHMBP2, LAS1L, PLEKHG5, SIGMAR1, SLC5A7, TRPV4, TRIP4, UBA1, VAPB | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Lung combo panel - IHC (ALK D5F3, ROS1) & RTPCR (BRAF V600E, EGFR[Hot Spot] exons 18, 19, 20, 21) | Oncology | 7 working days | Provide histopathological report of patient. Tumor content must be specified. | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC & RT-PCR |
| Acute Lymphoild Leukemia(ALL), 6 Markers, FISH | Oncology | 6 working days | Bone Marrow morphology report & Complete blood count report if available should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| Adenomatous polyposis coli (APC) gene analysis | Oncology | 21 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Next Generation Sequencing |
| AML Advance panel [(PML/Rara, bcr/abl, AML/ETO,Inv16) by RT-PCR (FLT3, NPM1, C-kit) by NGS] | Oncology | 14 working days | Not Available | Peripheral blood / bone marrow aspirate | EDTA anticoagulated peripheral blood / Bone marrow Aspirate in EDTA | 2-8℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | RT-PCR |
| AML Advance panel [(PML/Rara, bcr/abl, AML/ ETO,Inv16) by RT-PCR (FLT3, NPM1, C-kit) by NGS & Karyotyping] | Oncology | 14 working days | Not Available | Peripheral blood / bone marrow aspirate | EDTA anticoagulated peripheral blood???& Blood in Sodium Heparin Green Top(for FISH)/ Bone marrow As | 2-8℃ / 20-25℃ for Karyotyping | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | RT-PCR & Karyotyping |
| AML Basic panel [(PML/Rara, bcr/abl, AML/ETO, Inv16) by RT-PCR, (FLT3, NPM1) by NGS] | Oncology | 14 working days | Not Available | Peripheral blood / bone marrow aspirate | EDTA anticoagulated peripheral blood / Bone marrow Aspirate in EDTA | 2-8℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | RT-PCR |
| AML Comprehensive Panel [(PML/Rara, bcr/abl, AML/ETO, inv16 by RT-PCR) , (FLT3, NPM1, CEBPA & C-Kit by NGS)] | Oncology | 14 working days | Not Available | Peripheral blood / bone marrow aspirate | EDTA anticoagulated peripheral blood / Bone marrow Aspirate in EDTA | 2-8℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | Next generation Sequencing & RT-PCR |
| AML Comprehensive panel [(PML/Rara, bcr/abl, AML/ETO, inv16 by RT-PCR) , (FLT3, NPM1, CEBPA & C-Kit by NGS)] & Karyotyping | Oncology | 14 working days | Not Available | Peripheral blood / bone marrow aspirate | EDTA anticoagulated peripheral blood???& Blood in Sodium Heparin Green Top(for FISH)/ Bone marrow As | 2-8℃ / 20-25℃ for Karyotyping | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | Next generation Sequencing, Rt-PCR & Karyotyping |
| B MRD | Oncology | 2 working days | Provide detailed clinical history along with previous Flow Report | Bone marrow in EDTA | K2/K3 - EDTA Lavender top | 2-8℃ | 2.5-3ml of bone marrow in EDTA | Flowcytometry |
| BRAF V600 mutation analysis | Oncology | 7 working days | Provide histopathological report of patient. Tumor content must be specified. | FFPE blocks/slides/curls | FFPE blocks/slides in a cardboard box, FFPE curls in 1.5ml sterile tube | 20-25℃ | Minimum of 2 FFPE slides. Minimum of 2 FFPE curls each of 20 microns. Minimum of 10% (as assessed by | RT-PCR |
| BRCA1 & BRCA2 deletion/duplication analysis | Oncology | 14 working days | Provide histopathological report of patient (in primary cases) and relevant family history in case of first line relative screening | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | EDTA anticoagulated peripheral blood; DNA (RNAse treated) in sealed Eppendorf tube | MLPA |
| BRCA1 & BRCA2 gene analysis | Oncology | 21 working days | Provide histopathological report of patient (in primary cases) and relevant family history in case of first line relative screening | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Next Generation Sequencing |
| BRCA1 & BRCA2 somatic mutation testing | Oncology | 28 working days | Clinical diagnosis, Histopathology report is a mandatory requirement | FFPE blocks | Cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing |
| Carney complex (PRKAR1A) gene analysis | Oncology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Chromosomal breaks | Oncology | 15 working days | Not Available | Peripheral Blood | Sodium heparin-Green top | 20-25℃ | Minimum 4 ml peripheral blood | Cytogenetics/Karyotyping |
| Chronic Lymphoid Leukemia panel (4 markers-Del 17p,Trisomy 11, trisomy 12 and del 13q), FISH | Oncology | 6 working days | 17p deletion,trisomy11,trisomy 12,13q deletion Bone Marrow morphology report &Complete blood count report should accompany the sample(If available) | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| Chronic Lymphoid Leukemia Panel (5 markers-Del 6q, del 11q -ATM deletion, Trisomy 12,del 13q,del 17q | Oncology | 6 working days | Deletion 6q;Trisomy 11;Trisomy 12;Deletion 13;Deletion 17Bone Marrow morphology report &Complete blood count report if available should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| Chronic Myeloid Leukemia(CML), (4 markers- BCR-ABL,Iso 17q,del 7 and trisomy 8)FISH | Oncology | 6 working days | The markers include BCR-ABL Translocation, iso 17q, Deletion 7and Trisomy 8Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| Colorectal Basic Panel by NGS & IHC [KRAS, NRAS, BRAF by NGS and MMR by IHC] | Oncology | 14 working days | Not Available | Peripheral blood / bone marrow aspirate | EDTA anticoagulated peripheral blood / Bone marrow Aspirate in EDTA | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | Next Generation Sequencing & IHC |
| Colorectal cancer - Theranostic Panel (Hot Spot) | Oncology | 28 working days | KRAS, NRAS, HRAS, BRAF, PIK3CA, AKT1, PTEN & SMAD4Histopathology report must accompany the specimen Histopathology report must accompany the specimen | FFPE blocks | Cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing |
| Comprehensive molecular work-up for CLL Prognostication [NGS,Sanger,FISH] | Oncology | 21 working days | Inclusive tests are: MGM499-Comprehensive Leukemia Panel-57 geneMGM497-FISH for Deletion 17p(TP53), CLLMGM1342-IGHV gene mutation analysis | Peripheral blood / bone marrow aspirate | EDTA anticoagulated peripheral blood???& Blood in Sodium Heparin Green Top(for FISH);? | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate | Next Generation Sequencing,FISH,Sanger Sequencing |
| Comprehensive tumor panel (170 genes) | Oncology | 21 working days | Covers the HOTSPOT & point mutations as well as CNVs, indels and known gene fusions in the key oncogenes/tumor suppressor genes indicated in different tumor types. Please refer to the comprehensive tumor panel (170 genes) brochure and the liquid biopsy sample collection instructions for more details. Confirmatory clinical diagnosis of malignancy is a mandatory requirement. Additionally, we require histopathology report for solid tumors, bone marrow aspiration/blood smear report for hematological malignancies, treatment history and latest PET-CT report for liquid biopsy | FFPE Block | FFPE block in cardboard box | 20-25℃ | FFPE block with a minimum of 10% (as assessed by the pathologist) of tumor cells should be present | Next Generation Sequencing |
| DPYD IVS14+1G>A mutation analysis | Oncology | 7 working days | Dihydropyrimidine dehydrogenase deficiency evaluation in patients with 5-fluorouracil (5FU) or capecitabine toxicity | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Sanger sequencing |
| EGFR (T790M, L858R, exon 19 deletion) screening by ddPCR | Oncology | 5 working days | T790M, L858R, exon 19 deletion | FFPE Block/peripheral blood in Streck tubes (for liquid biopsy) | FFPE block in cardboard box; peripheral blood in 2 Streck tubes | 20-25℃ | FFPE block with a minimum of 5% (as assessed by the pathologist) of tumor cells should be present; 2 | Droplet Digital PCR |
| EGFR gene analysis (Hot Spot) - 4 exons (18, 19, 20, 21) | Oncology | 4 working days | Provide histopathological report of patient (in primary cases) Includes T790M | FFPE blocks/slides/curls | FFPE blocks/slides in a cardboard box, FFPE curls in 1.5ml sterile tube | 20-25℃ | Minimum of 2 FFPE slides. Minimum of 2 FFPE curls each of 20 microns. Minimum of 10% (as assessed by | RT-PCR |
| EGFR T790M mutation screening by ddPCR | Oncology | 5 working days | T790M | FFPE Block/peripheral blood in Streck tubes (for liquid biopsy) | FFPE block in cardboard box; peripheral blood in 2 Streck tubes | 20-25℃ | FFPE block with a minimum of 5% (as assessed by the pathologist) of tumor cells should be present; 2 | Droplet Digital PCR |
| FIP1L1-PDGFRA gene re-arrangement | Oncology | 5 working days | Not Available | Peripheral blood/bone marrow aspirate | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA | Room temperature (refrigerate overnight if necessary) | Minimum 4ml of peripheral blood; minimum 1ml of bone marrow aspirate | RT-PCR |
| FISH for Deletion 5/5q (5q31,5q33), MDS/AML | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for Inv(3) (MECOM, 3q26) gene rearrangement, MDS/AML | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for PML-RARA t(15;17)(q24,q21), AML | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for 1p19q co-deletion,1p3619q13 | Oncology | 7 working days | Provide detailed clinical history on the Lab test request form and histopathology reports along with slides. | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | FISH |
| FISH for 6q deletion, CLL | Oncology | 6 working days | Bone Marrow morphology report & Complete blood count report if available should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for ALK and ROS-1 gene rearrangement , Lung cancer | Oncology | 6 working days | Provide detailed clinical history on the Lab request form and histopathology reports along with slides | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | FISH |
| FISH for ALk(2p23) gene rearrangement, NSCLC | Oncology | 7 working days | Provide detailed clinical history on the Lab test request form and histopathology reports along with slides | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | FISH |
| FISH for ALL Panel (4 markers-E2A Breakapart, t(12;21), BCR-ABL, MLL) | Oncology | 6 working days | Includes E2A Break apart, t(12;21), BCR-ABL, MLL;Bone Marrow morphology report & Complete blood count report should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for ALL Panel | Oncology | 8 working days | MLL, iAMP21/ETV6-RUNX1, TCRA/D,BCR-ABL,C-Myc, IGHBA, E2A BreakapartBone Marrow morphology report & Complete blood count report should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| SH for AML panel | Oncology | 6 working days | Includes t(8;21)(q22;q22), t(15;17)(q24;21), inv(16) or t(16;16), inv3, Del 5q, Del 7q, MLL amplification, BCR/ABL t(9;22) fusion. Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheralblood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for AML panel (All markers(8)) | Oncology | 7 working days | Includes t(8;21)(q22;q22), t(15;17)(q24;21), inv(16) or t(16;16), inv 3, Del 5q, Del 7q, MLL amplification, BCR/ABL t(9;22) fusion. Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for BCR-ABL t(9;22)(q34;q11.2), AML/CML/MPN | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for CLL Panel (All markers- Del6q, Del 17p, Del13q,ATM deletion/trisomy 11, Trisomy 12, IGH rea | Oncology | 7 working days | Del6q, Del 17p, Del13q,ATM deletion/trisomy 11, Trisomy 12, IGH rearrangement Bone Marrow morphology report & Complete blood count report should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for C-MYC (8q24) Translocation, ALL | Oncology | 6 working days | Bone Marrow morphology report & Complete blood count report if available should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for C-MYC (8q24) Translocation, Multiple Myeloma [With Plasma cell Enrichment] | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings(mandatory). All samples for FISH | Bone marrow aspirate | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | FISH |
| FISH for del20q , MDS/AML | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for deletion 13q(13q14.2, 13q34), CLL | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for deletion 13q(13q14.2, 13q34), MM [With Plasma cell Enrichment] | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings(mandatory). All samples for FISH | Bone marrow aspirate | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | FISH |
| FISH for Deletion 17p(TP53), CLL | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for Deletion 17p(TP53), Multiple Myeloma [With Plasma cell Enrichment] | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings(mandatory). All samples for FISH | Bone marrow aspirate | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | FISH |
| FISH for E2A (19p13.3) Translocation, ALL | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for ERBB2(HER2) gene amplification, Breast cancer | Oncology | 7 working days | Her2-neu fixation timings and type of fixative has to be recorded. Histopath report, IHC report and IHC slide (if IHC testing is done) should be sent along with the Test Request Form | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | FISH |
| FISH for ETV6-RUNX1 t(12;21)(p13;q22), ALL | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for iAMP21,ALL | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for IGH (14q32) Gene rearrangement, CLL | Oncology | 6 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should ac | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for IGH (14q32) Gene rearrangement, Multiple Myeloma [With Plasma cell Enrichment] | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings(mandatory). All samples for FISH | Bone marrow aspirate | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 3ml of peripheral blood | FISH |
| FISH for IGH /MAF t(14;16)(q32;q23), Multiple Myeloma [With Plasma cell Enrichment] | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings(mandatory). BMA morphology is mandatory. All samples for FISH to reach the lab with in 24 hours of collection for best results. | Bone marrow aspirate | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for IGH/CCND1 t(11;14)(q13;q32), Multiple Myeloma [With Plasma cell Enrichment] | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings(mandatory). BMA morphology is mandatory. All samples for FISH to reach the lab with in 24 hours of collection for best results. | Bone marrow aspirate | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for IGH/FGFR3 t(4;14)(p16;q32), Multiple Myeloma [With Plasma cell Enrichment] | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings(mandatory). BMA morphology is mandatory. All samples for FISH to reach the lab with in 24 hours of collection for best results. | Bone marrow aspirate | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for inv(16)/t(16;16)(p13.1;q22), AML | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for iso 17q, CML | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for MDS ( 4 markers ) | Oncology | 6 working days | Includes Del 5q, Del 7q, Del 20q, Trisomy 8Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for MDS (All markers (8)) | Oncology | 7 working days | Includes Deletion 5q, Deletion 7q, Deletion 20q, C-mycamplifications/trisomy 8, Inv 3, MLL Amplification, 17p deletion,13q deletion Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for MDS/AML (6 markers- Del 5/5q, Del 7/7q, Trisomy 8, RUNX-RUNX1 t(8;21), PML-RARA t(15;17), I | Oncology | 7 working days | Includes Del 5/5q, Del 7/7q, Trisomy 8, RUNX-RUNX1 t(8;21),PML-RARA t(15;17), Inv(16);Bone Marrow morphology report & Complete blood count report should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for MLL(11q23) amplification, AML/MLL/MDS | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for MPN panel (3 markers- BCR/ABL, PDGFRA, PDGFRB) | Oncology | 6 working days | BCR/ABL, PDGFRA, PDGFRBBone Marrow morphology report & Complete blood count report should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for MPN panel (5 markers- BCR/ABL, PDGFRA, PDGFRB, JAK2 and FGFR1 gene rearrangements) | Oncology | 7 working days | Includes BCR/ABL, PDGFRA, PDGFRB, JAK2 and FGFR1 gene rearrangements. Bone Marrow morphology report & Complete blood count report should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for Multiple Myeloma (5 markers) | oncology | 6 working days | Inclusive tests:t(11;14) - IGH/CCND1;FISH for t(4;14)/FGFR3/IGH;FISH for t(14;16)/IGH/MAF;FISH for 13q deletion; FISH for 17p deletion Provide detailed clinical history along with bone marrow findings(mandatory). BMA morphology is mandatory. All samples for FISH to reach the lab with in 24 hours of collection for best results. | Bone marrow aspirate | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for PDGFRA(4q12) gene rearrangement, MPN | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for PDGFRB (5q32-33) gene rearrangement, MPN | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for ROS-1 (6q22.1) rearrangement, NSCLC | Oncology | 7 working days | Provide detailed clinical history on the Lab test request form and histopathology reports along with slides | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | FISH |
| FISH for RUNX-RUNX1 t(8;21)(q22;q22), AML | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for TCRA/D (14q11.2) gene rearrangement, ALL | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for Trisomy 11, CLL | Oncology | 6 working days | Bone Marrow morphology report & Complete blood count report if available should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for Trisomy 12, CLL | Oncology | 6 working days | Bone Marrow morphology report & Complete blood count report if available should accompany the sample | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for Trisomy 8 /c-myc amplification, MDS/AML/ALL | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| GIST (Gastrointestinal Stromal Tumor) - Theranostic Panel (Hot Spot) | Oncology | 21 working days | BRAF, KIT & PDGFRA Histopathology report must accompany the specimen | FFPE blocks | Cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing |
| Hereditary cancer gene panel - focussed | Oncology | 21 working days | AIP, ALK, APC, AR, ATM, BAP1, BARD1, BLM, BMPR1A, BRCA1, BRCA2, BRIP1, BUB1B, CD82, CDC73, CDH1, CDK4, CDKN1C, CDKN2A, CEBPA, CEP57, CHEK2, CYLD, DDB2, DICER1, DIS3L2, EGFR, ELAC2, ENG, EPCAM, ERCC2, ERCC3, ERCC4, ERCC5, EXT1, EXT2, EZH2, FANCA, FANCB, FANCC, FANCD2, FANCE, FANCF, FANCG, FANCI, FANCL, FANCM, FH, FLCN, GATA2, GPC3, HRAS, KIT, MAX, MEN1, MET, MLH1, MLH3, MRE11A, MSH2, MSH3, MSH6, MSR1, MUTYH, MXI1, NBN, NF1, NF2, NSD1, PALB2, PHOX2B, PMS1, PMS2, PRF1, PRKAR1A, PTCH1, PTEN, RAD50, RAD51C, RAD51D, RB1, RECQL4, RET, RHBDF2, RNASEL, RUNX1, SBDS, SDHAF2, SDHB, SDHC, SDHD, SLX4, SMAD4, SMARCB1, STK11, SUFU, TGFBR2, TMEM127, TP53, TSC1, TSC2, VHL, WRN, WT1, XPA, XPC | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Next Generation Sequencing |
| IGHV gene mutation analysis | Oncology | 14 working days | Bone Marrow morphology report, Complete blood count report and/or FISH report if available should accompany the sample | Peripheral blood / bone marrow aspirate / Purified genomic DNA | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed eppendorf tube? | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Sanger Sequencing |
| Imatinib resistance (ABL kinase) gene analysis - IRMA | Oncology | 10 working days | ABL1 | Peripheral blood/RNA | EDTA tube anticoagulated peripheral blood; RNA in sealed Eppendorf tube | Room temperature (refrigerate overnight if necessary) | 4ml of Peripheral blood; 1?g of RNA | Next Generation Sequencing |
| KIT gene analysis - 4 exons (9, 11, 13, 17) | Oncology | 10 working days | Provide histopathological report of patient | FFPE blocks/slides/curls | FFPE blocks/slides in a cardboard box, FFPE curls in 1.5ml sterile tube | 20-25℃ | Minimum of 2 FFPE slides. Minimum of 2 FFPE curls each of 20 microns. Minimum of 30% (as assessed by | Next generation Sequencing |
| KRAS gene analysis (Hot Spot) | Oncology | 5 working days | Provide histopathological report of patient | FFPE blocks/slides/curls | FFPE blocks/slides in a cardboard box, FFPE curls in 1.5ml sterile tube | 20-25℃ | Minimum of 2 FFPE slides. Minimum of 2 FFPE curls each of 20 microns. Minimum of 10% (as assessed by | RT-PCR |
| Lung Advanced Panel by NGS & IHC [EGFR, ALK, ROS1, BRAF, MET (SNVs, Indels, Skipping mutations), RET, Her2 by NGS & PDL1 by IHC] | Oncology | 14 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing & IHC |
| Lung Advanced Panel by NGS [EGFR, ALK, ROS1, BRAF,MET (SNVs,Indels,Skipping mutations), RET, Her2] | Oncology | 14 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing |
| Lung Basic Panel by NGS & IHC [EGFR, ALK, ROS1, BRAF,MET (SNVs & Indels) by NGS & PDL1 by IHC] | Oncology | 14 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing & IHC |
| Lung Basic Panel by NGS [EGFR, ALK, ROS1, BRAF,MET (SNVs & Indels)] | Oncology | 14 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing |
| Lung Comprehensive Panel [EGFR, ALK, ROS1, BRAF, MET (SNVs, Indels, Skipping mutations), RET, Her2 by NGS, PDL1 by IHC & MSI by Fragment Analysis] | Oncology | 14 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing , IHC & Fragment Analysis |
| Lynch syndrome (HNPCC) - (MLH1, MSH2, EPCAM) deletion/duplication analysis | Oncology | 14 working days | Provide histopathological report of patient | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | MLPA |
| Lynch Syndrome/HNPCC gene panel | Oncology | 21 working days | MLH1, MSH2, MSH6, PMS1, EPCAM, MSH3, MLH3, PMS2 | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Next Generation Sequencing |
| MGMT gene methylation analysis (Temozolomide Resistance) | Oncology | 14 working days | Provide histopathological report of patient (in primary cases) | FFPE blocks/slides/curls | FFPE blocks/slides in a cardboard box, FFPE curls in 1.5ml sterile tube | 20-25℃ | Minimum of 2 FFPE slides. Minimum of 2 FFPE curls each of 20 microns. Minimum of 10% (as assessed by | RT-PCR |
| MSI by fragment analysis | Oncology | 7 working days | NCI Bathesda MSI Markers (BAT25, BAT26, D2123, D5346, D17S250) | Peripheral blood, FFPE blocks | EDTA anticoagulated peripheral blood; FFPE blocks in a cardboard box | 20-25℃ | Minimum 4ml of peripheral blood; Minimum 30% (as assessed by the pathologist) of tumor tissue should | Fragment analysis |
| Multiplex RT-PCR panel for Leukemia(28 translocations) | Oncology | 5 working days | Provide clinical diagnosis; Includes following translocations:del1(p32), t(1;11)(MLL-EPS15), t(1;11)(MLL-MLLT11), t(1;19),t(3;5), t(3;21), t(4;11), t(5;12), t(5;17), t(6;9), t(6;11), t(8;21), t(9;9),t(9;11), t(9;12), t(9,22), t(10;11), t(11;17)(MLL-MLLT6), t(11;17)(ZBTB16-RARA), t(11;19)(MLL-ELL), t(11;19)(MLL-MLLT1),t(12;21), t(12;22), t(15;17), inv(16), t(16;21), t(17;19), t(X;11), | Peripheral blood/bone marrow aspirate | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA | Room temperature (refrigerate overnight if necessary) | Minimum 4ml of peripheral blood; minimum 1ml of bone marrow aspirate | RT-PCR |
| Myeloma Panel - Flowcytometry (CD45, CD38, CD19, CD56, CD138, kappa, lambda) | Oncology | 2 working days | Appropriately labelled air-dried and unstained Bone marrow aspirate smears and Peripheral blood smears must accompany every specimen. | Peripheral blood along with bone marrow aspirate in EDTA | Bone marrow smears on slides; bone marrow aspirate in EDTA | 2-8℃ | Minimum of 2 bone marrow smears; minimum 1ml of bone marrow aspirate | Flowcytometry |
| Myeloma Panel (4 markers),FISH | Oncology | 6 working days | Includes C-myc(8q24.21) rearrangement, Del 13q,IGH(14q32) translocation, Del 17pProvide detailed clinical history along with bone marrow findings(mandatory). BMA morphology is mandatory. All samples for FISH to reach the lab with in 24 hours of collection for best results. Inclusive tests are IGH translocation;13q deletion;17p deletion, Cmyc re-arrangement | Bone marrow aspirate | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| Non Small cell Lung Cancer (NSCLC) NGS Panel (Hot Spot) | Oncology | 21 working days | ALK, BRAF, EGFR, ERBB2, MET, PIK3CA, RET, KRAS, NRAS,PTEN, AKT1, DDR2, HRAS, and MAP2K1Histopathology report must accompany the specimen | FFPE blocks | Cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing |
| NRAS gene analysis (Hot Spot) | Oncology | 5 working days | Provide histopathological report of patient (in primary cases) | FFPE blocks/slides/curls | FFPE blocks/slides in a cardboard box, FFPE curls in 1.5ml sterile tube | 20-25℃ | Minimum of 2 FFPE slides. Minimum of 2 FFPE curls each of 20 microns. Minimum of 10% (as assessed by | RT-PCR |
| OncoFocus - ct DNA for EGFR | Oncology | 12 working days | includes HOTSPOT mutations in EGFR (Exons 18, 19, 20, 21; includes T790M) | Peripheral blood | Peripheral blood in 2 Streck tubes provided by Lab | 20-25℃ | 10ml in each tube (strictly) | Next Generation Sequencing |
| OncoFocus Express - ct DNA for EGFR | Oncology | 7 working days | includes HOTSPOT mutations in EGFR (Exons 18, 19, 20, 21; includes T790M) | Peripheral blood | Peripheral blood in 2 Streck tubes provided by Lab | 20-25℃ | 10ml in each tube (strictly) | Next Generation Sequencing |
| OncoSelect ctDNA for EGFR T790M and C797S | Oncology | 12 working days | HOTSPOT mutations in EGFR (T790M - indicating resistance to first & second gen TKI and C797S indicating resistance to third gen TKIs) Primary use in Adenocarcinoma - Lung | Peripheral blood | Peripheral blood in 2 Streck tubes provided by Lab | 20-25℃ | 10ml in each tube (strictly) | Next Generation Sequencing |
| OncoTrack - ct DNA for Hot Spot mutations in 4 genes (EGFR, KRAS, NRAS, BRAF) | Oncology | 12 working days | HOTSPOT mutations in EGFR (Exons 18, 19, 20, 21; includes T790M), KRAS (Exons 2, 3, 4), NRAS (Exons 2, 3, 4),BRAF (V600E) | Peripheral blood | Peripheral blood in 2 Streck tubes provided by Lab | 20-25℃ | 10ml in each tube (strictly) | Next Generation Sequencing |
| PDGFRA gene analysis - 3 exons (12, 14, 18) | Oncology | 10 working days | Provide histopathological report of patient (in primary cases) | Peripheral blood/bone marrow aspirate/purified genomic DNA/FFPE blocks/slides/curls | EDTA anticoagulated peripheral blood; bone marrow aspirate in EDTA; DNA in sealed Eppendorf tube; FF | 20-25℃ | Minimum 4ml of peripheral blood; minimum 1ml of bone marrow aspirate; minimum 1 microgram of DNA (co | Next Generation Sequencing |
| PNH by FLAER- High Sensitivity | Oncology | 2 working days | Provide detailed clinical history along with CBC reports | Peripheral blood in EDTA | Two K2/K3 - EDTA Lavender top | 2-8℃ | 2.7 mL Each | Flowcytometry |
| RB1 gene analysis (germline) | Oncology | 21 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| RB1 gene deletion/duplication analysis | Oncology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Retinoblastoma gene 13q14 region by FISH | Oncology | 7 working days | Not Available | Bone marrow aspirate | Sodium heparin-Green top | 20-25℃ | Minimum 2 ml of bone marrow aspirate | FISH |
| Somatic Cancer Mutation Panel / Hot Spot tumor panel | Oncology | 21 working days | Provide histopathological report of patient. Inclusive genes:ABL1, AKT1, ALK, APC, ATM, BRAF (inclusive of v600E), CDH1, CDKN2A, CSF1R, CTNNB1, DDR2, DNMT3A, EGFR, ERBB2, ERBB4, EZH2, FBXW7, FGFR1, FGFR2, FGFR3, FLT3, FOXL2, GNA11, GNAQ, GNAS, HNF1A, HRAS, IDH1, IDH2, JAK2, JAK3, KDR, KIT, KRAS, MAP2K1/MEK1, MET, MLH1, MPL, MSH6, NOTCH1, NPM1, NRAS, PDGFRA, PIK3CA, PTEN, PTPN11, RB1, RET, SMAD4, SMARCB1, SMO, SRC, STK11, TP53, TSC1,VHLExcept for TP53 only specific hotspots are covered in the aforementioned genes, that is, those which are therapeutically relevant. Specific exonic coverage will be provided on individual reports | FFPE blocks | Cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing |
| T- MRD | Oncology | 2 working days | Provide detailed clinical history along with previous Flow Report (Mandatory-Sample will not be accepted without previous Flowcytometry report) | Bone marrow in EDTA | K2/K3 - EDTA Lavender top | 2-8℃ | 6mL (2 tubes atleast 3ml each) | Flowcytometry |
| TP53 gene deletion/duplication analysis | Oncology | 14 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | MLPA |
| Von Hippel-Lindau syndrome (VHL) gene analysis | Oncology | 21 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 4ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Next Generation Sequencing |
| Oncotrack - Ultima [Liquid biopsy for 56 theranostic genes] | Oncology | 21 working days | Provide histopathological report of patient. Inclusive genes:ABL1, AKT1, ALK, APC, ATM, BRAF (inclusive of v600E), CDH1,CDKN2A, CSF1R, CTNNB1, DDR2, DNMT3A, EGFR, ERBB2,ERBB4, EZH2, FBXW7, FGFR1, FGFR2, FGFR3, FLT3, FOXL2,GNA11, GNAQ, GNAS, HNF1A, HRAS, IDH1, IDH2, JAK2, JAK3,KDR, KIT, KRAS, MAP2K1/MEK1, MET, MLH1, MPL, MSH6,NOTCH1, NPM1, NRAS, PDGFRA, PIK3CA, PTEN, PTPN11,RB1, RET, SMAD4, SMARCB1, SMO, SRC, STK11, TP53, TSC1,VHLExcept for TP53 only specific hotspots are covered in the aforementioned genes, that is, those which are therapeutically relevent. Specific exonic coverage will be provided on individual reports | Peripheral blood | Peripheral blood in 2 Streck tubes provided by Lab | 20-25℃ | 10ml in each tube (strictly) | Next Generation Sequencing |
| ALK D5F3 analysis | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| Breast Prognostic/predictive IHC2 panel (ER, PR) | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| Breast Prognostic/predictive IHC3 panel (ER, PR, Her2/neu) | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| c-MET IHC analysis | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| ER IHC Analysis | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| Her 2 Gastric tissue | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| Her2/neu IHC Analysis | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| Lung tumor panel I (ALK D5F3, ROS1, c-MET) | Oncology IHC | 6 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| Lung tumor panel II (ANY TWO OF - ALK D5F3, ROS1, c-MET) | Oncology IHC | 6 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| Lynch Syndrome Mismatch Repair (MMR) 4 gene (MLH1, MSH2, MSH6 & PMS2) panel - IHC[Microsatellite instability MSI] | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| MIB-1/Ki67 IHC Analysis | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| PDL1 IHC analysis | Oncology IHC | 7 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| PR IHC Analysis | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| Prognostic/predictive IHC4 panel (ER, PR, Her2/neu,MIB-1/Ki67) | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| ROS1 IHC analysis | Oncology IHC | 4 working days | Provide histopathological report of patient | FFPE blocks | cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | IHC |
| IDH1 & IDH2 gene analysis | Oncology/ Hemato-Oncoogy | 12 working days | Provide histopathological report for solid tumors; Bone Marrow morphology report, Complete blood count report and/or FISH report for leukemia | FFPE block for Solid tumors;Peripheral Blood/Purified Genomic DNA for Leukemia? | FFPE block in cardboard box; EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | FFPE block with a minimum of 10% (as assessed by the pathologist) of tumor cells should be present; | Next Generation Sequencing |
| C8orf37 gene sequencing | Ophthalmology | 21 working days | C8orf37 Associated with autosomal recessive cone-rod dystrophy (arCRD) and retinitis pigmentosa (arRP) | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Choroideremia (CHM) deletion/duplication analysis | Ophthalmology | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Congenital cataract gene panel | Ophthalmology | 21 working days | AGK, BFSP1, BFSP2, CHMP4B, CRYAA, CRYAB, CRYBA1, CRYBA2, CRYBA4, CRYBB1, CRYBB2, CRYBB3, CRYGB, CRYGC, CRYGD, CRYGS, CTDP1, EPHA2, FAM126A, FOXE3, FTL, FYCO1, GALK1, GCNT2, GFER, GJA3, GJA8, HSF4, LEMD2, LIM2, LSS, MAF, MIP, MSMO1, NHS, P3H2, PITX3, RDH11, SLC16A12, SLC33A1, TDRD7, UNC45B, VIM, WFS1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Congenital stationary night blindness gene panel | Ophthalmology | 21 working days | CACNA1F, GNAT1, GNB3, GPR179, GRK1, GRM6, LRIT3, NYX, PDE6B, RDH5, RHO, RPE65, SAG, SLC24A1, TRPM1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Corneal dystrophy gene panel | Ophthalmology | 21 working days | AGBL1, APOA1, CHST6, COL8A2, DCN, KERA, KRT12, KRT3, OVOL2, PAX6, PIKFYVE, PITX2, PRDM5, PXDN, SLC4A11, TACSTD2, TCF4, TGFBI, UBIAD1, ZEB1, ZNF469 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Leber congenital amaurosis gene panel | Ophthalmology | 21 working days | AIPL1, CEP290, CRB1, CRX, GDF6, GUCY2D, IMPDH1, IQCB1, KCNJ13, LCA5, LRAT, NMNAT1, PRPH2, RD3, RDH12, ROM1, RPE65, RPGRIP1, SPATA7, TULP1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Optic atrophy gene panel | Ophthalmology | 21 working days | ACO2, OPA1, OPA3, RTN4IP1, TMEM126A, YME1L1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Retinal degeneration gene panel | Ophthalmology | 21 working days | ABCA4, ABHD12, ACBD5, ACO2, ADAM9, ADAMTS18, AHI1, AIPL1, ALMS1, ARL2BP, ARL6, ATF6, ATOH7, BBIP1, BBS1, BBS1, BBS12, BBS2, BBS4, BBS5, BBS7, BBS9, BEST1, C1QTNF5, C2ORF197, C21orf2, C2orf71, C8orf37, CA4, CABP4, CACNA1F, CACNA2D4, CAPN5, CC2D2A, CCDC28B, CDH23, CDH3, CDHR1, CEP164, CEP25, CEP29, CERKL, CFH, CHM, CIB2, CLN3, CLRN1, CNGA1, CNGA3, CNGB1, CNGB3, CNNM4, COG4, COG6, COL11A1, COL2A1, COL9A1, CRB1, CRX, CSPP1, CYP4V2, DFNB31, DHDDS, DHX38, DRAM2, DTHD1, EFEMP1, ELOVL4, EMC1, EYS, FAM161A, FBLN5, FLVCR1, FSCN2, FZD4, GDF6, GNAT1, GNAT2, GNPTG, ADGRA3, GPR179, ADGRV1, GRK1, GRM6, GUCA1A, GUCA1B, GUCY2D, HARS, HGSNAT, HK1, HMCN1, IDH3B, IFT14, IFT172, IFT27, IMPDH1, IMPG1, IMPG2, INPP5E, IQCB1, ITM2B, JAG1, KCNJ13, KCNV2, KIAA1549, KIF11, KLHL7, LAMA1, LCA5, P3H2, LRAT, LRIT3, LRP5, LZTFL1, MAK, MERTK, MFRP, MKKS, MKS1, MVK, MYO7A, NDP, NEK2, NEUROD1, NMNAT1, NPHP1, NPHP4, NR2E3, NR2F1, NRL, NYX, OAT, OFD1, OPA1, OPA3, OTX2, PANK2, PAX2, PAX6, PCDH15, PCYT1A, PDE6A, PDE6B, PDE6C, PDE6G, PDE6H, PDZD7, PGK1, PITPNM3, PLA2G5, PLK4, PNPLA6, POC1B, PRCD, PROM1, PRPF3, PRPF31, PRPF4, PRPF6, PRPF8, PRPH2, PRPS1, RAB28, RAX2, RB1, RBP3, RBP4, RCBTB1, RD3, RDH11, RDH12, RDH5, RGR, RGS9, RGS9BP, RHO, RIMS1, RLBP1, ROM1, RP1, RP1L1, RP2, RP9, RPE65, RPGR, RPGRIP1, RPGRIP1L, RS1, SAG, SDCCAG8, SEMA4A, SLC24A1, SLC38A8, SLC7A14, SNRNP2, SPATA7, SPP2, TEAD1, TIMP3, TMEM126A, TMEM216, TMEM67, TOPORS, TREX1, TRIM32, TRNT1, TRPM1, TSPAN12, TTC8, TTLL5, TTPA, TUB, TUBGCP4, TUBGCP6, TULP1, UNC119, USH1C, USH1G, USH2A, VCAN, WDPCP, WDR19, ZNF48, ZNF513 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Usher syndrome gene panel | Ophthalmology | 21 working days | CDH23, CIB2, CLRN1, DFNB31, ADGRV1, HARS, MYO7A, PCDH15, PDZD7, USH1C, USH1G, USH2A | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Amniotic Fluid karyotyping + FISH (5 probes - 13,18,21, sex chromosome) | Prenatal | 15 working days | Not Available | Amniotic Fluid | Amniotic fluid in 2 sterile falcon tubes | 20-25℃ | 2 tubes with 10ml in each sterile tube | Cytogenetics/Karyotyping + FISH |
| Amniotic Fluid karyotyping + FISH(2 probes)(either 13/21 or 18/X/Y] | Prenatal | 15 working days | Not Available | Amniotic Fluid | Amniotic fluid in 2 sterile falcon tubes | 20-25℃ | 2 tubes with 10ml in each sterile tube | Cytogenetics/Karyotyping + FISH |
| Carrier screening - Gold [500 genes NGS & MLPA (SMA, DMD, CYP21A2)] | Prenatal | 21 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Next Generation Sequencing & MLPA |
| Carrier screening - Platinum [~2000 recessive genes included in clinical exome & MLPA (SMA, DMD, CYP | Prenatal | 14 working days | Carrier test Platinum involves next generation sequencing of clinically relevant genes, reported in | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Next Generation Sequencing & MLPA |
| Carrier screening - Platinum [2000 recessive genes included in clinical exome & MLPA (SMA, DMD, CYP21A2) ] | Prenatal | 21 working days | Carrier test Platinum involves next generation sequencing of clinically relevant genes, reported in either OMIM or HGMD to be associated with a Mendelian disorder. The custom design provides greater than or equal to 98% coverage of around 2000 recessive genes, with a mean on target read depth of 80-100x. | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Next Generation Sequencing & MLPA |
| Carrier screening - Silver [100 genes NGS & MLPA (SMA, DMD, CYP21A2)] | Prenatal | 21 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Next Generation Sequencing & MLPA |
| Cord blood karyotyping + FISH (2 probes)(either 13/21 or 18/X/Y) | Prenatal | 8 working days | Not Available | Cord Blood | Sodium heparin-Green top | 20-25℃ | 1.5 to 2 ml | Cytogenetics/Karyotyping + FISH |
| Cord Blood karyotyping + FISH (5 probes - 13, 18, 21, sex chromosomes) | Prenatal | 8 working days | Not Available | Cord Blood | Sodium heparin-Green top | 20-25℃ | 1.5 to 2 ml | Cytogenetics/Karyotyping + FISH |
| Cord Blood karyotyping only | Prenatal | 8 working days | Not Available | Cord Blood | Sodium heparin-Green top | 20-25℃ | 1.5 to 2 ml | Cytogenetics/Karyotyping |
| Cord Blood Procedure + Karyotyping | Prenatal | 8 working days | Not Available | Cord Blood | Sodium heparin-Green top | 20-25℃ | 1.5 to 2 ml | Cytogenetics/Karyotyping |
| Cord Blood Procedure + Karyotyping + FISH (5 probes - 13, 18, 21, sex chromosomes) | Prenatal | 8 working days | Not Available | Cord Blood | Sodium heparin-Green top | 20-25℃ | 1.5 to 2 ml | Cytogenetics/Karyotyping + FISH |
| Cord Blood Procedure + Karyotyping+ FISH (2 probes)(either 13/21 or 18/X/Y) | Prenatal | 8 working days | Not Available | Cord Blood | Sodium heparin-Green top | 20-25℃ | 1.5 to 2 ml | Cytogenetics/Karyotyping + FISH |
| CVS karyotyping + FISH (2 probes) (either 13/21 or 18/X/Y) | Prenatal | 10 working days | Not Available | Chorionic Villus Sample(CVS) | CVS In a sterile 15ml falcon tube in provided medium | 20-25℃ | CVS 20 - 30mg | Cytogenetics/Karyotyping + FISH |
| CVS karyotyping + FISH (5 probes - 13,18,21, sex chromosomes) | Prenatal | 10 working days | Not Available | Chorionic Villus Sample(CVS) | CVS In a sterile 15ml falcon tube in provided medium | 20-25℃ | CVS 20 - 30mg | Cytogenetics/Karyotyping + FISH |
| CVS karyotyping only | Prenatal | 10 working days | Not Available | Chorionic Villus Sample(CVS) | CVS In a sterile 15ml falcon tube in provided medium | 20-25℃ | CVS 20 - 30mg | Cytogenetics/Karyotyping |
| Di George / VCF syndrome | Prenatal | 9 working days | Not Available | On all type of samples1. Peripheral blood2. POC - tissue3. Prenatal - Cord blood/Amniotic fluid/ | Blood/Cord blood- Sodium heparinPOC - Tissue in sterile containerAmniotic fluid - In 2 sterile fal | 20-25℃ | Blood/Cord blood- 2 mlAmniotic fluid - 5 ml in each tubeCVS - 20-30mg in provided medium | FISH |
| FISH (2 probes) (either 13/21 or18/X/Y) | Prenatal | 4 working days | Not Available | On all type of samples1. Peripheral blood2. POC - tissue3. Prenatal - Cord blood/Amniotic fluid/ | Blood/Cord blood- Sodium heparinPOC - Tissue in sterile containerAmniotic fluid - In 2 sterile fal | 20-25℃ | Blood/Cord blood- 2 mlAmniotic fluid - 5 ml in each tubeCVS - 20-30mg in provided medium | FISH |
| FISH (7 probes - 13,16,18,21,22, sex chromosome) | Prenatal | 4 working days | Not Available | On all type of samples1. Peripheral blood2. POC - tissue3. Prenatal - Cord blood/Amniotic fluid/ | Blood/Cord blood- Sodium heparinPOC - Tissue in sterile containerAmniotic fluid - In 2 sterile fal | 20-25℃ | Blood/Cord blood- 2 mlAmniotic fluid - 5 ml in each tubeCVS - 20-30mg in provided medium | FISH |
| FISH(5 probes-13,18,21,sex chromosomes) | Prenatal | 4 working days | Not Available | On all type of samples1. Peripheral blood2. POC - tissue3. Prenatal - Cord blood/Amniotic fluid/ | Blood/Cord blood- Sodium heparinPOC - Tissue in sterile containerAmniotic fluid - In 2 sterile fal | 20-25℃ | Blood/Cord blood- 2 mlAmniotic fluid - 5 ml in each tubeCVS - 20-30mg in provided medium | FISH |
| PGD by Sanger/PCR (1 variant) - per embryo | Prenatal | 14 working days | Pre-PGD passed for one variant | Day-3 (single cell) or day-5 (few cells) embryo biopsy Note: Day-5 biopsy is preferred | 0.2 ml PCR Tubes from the PGD Kit provided by Lab. Note: Please request for the PGD kit before | -20 to -80℃ (dry ice shipment). Please contact with the Lab prior to performing the biopsy. | Single cell(day-3) or few cells(day-5) embryo biopsy in 2.5 ul transport medium available in the Med | Sanger sequencing |
| PGD by Sanger/PCR (2 variants) - per embryo | Prenatal | 14 working days | Not Available | Day-3 (single cell) or day-5 (few cells) embryo biopsy Note: Day-5 biopsy is preferred | 0.2 ml PCR Tubes from the PGD Kit provided by Lab. Note: Please request for the PGD kit before | -20 to -80℃ (dry ice shipment). Please contact with the Lab prior to performing the biopsy. | Single cell(day-3) or few cells(day-5) embryo biopsy in 2.5 ul transport medium available in the Med | Sanger Sequencing |
| PGD by Sanger/PCR (3 variants) - per embryo | Prenatal | 14 working days | Not Available | Day-3 (single cell) or day-5 (few cells) embryo biopsy | 0.2 ml PCR Tubes from the PGD Kit provided by Lab. Note: Please request for the PGD kit before | -20 to -80℃ (dry ice shipment). Please contact with the Lab prior to performing the biopsy. | Single cell(day-3) or few cells(day-5) embryo biopsy in 2.5 ul transport medium available in the Med | Sanger Sequencing |
| PGD by Sanger/PCR (4 variants) - per embryo | Prenatal | 14 working days | Not Available | Day-3 (single cell) or day-5 (few cells) embryo biopsyNote: Day-5 biopsy??is preferred | 0.2 ml PCR Tubes from the PGD Kit provided by Lab. Note: Please request for the PGD kit before | -20 to -80℃ (dry ice shipment). Please contact with the Lab prior to performing the biopsy.℃ | Single cell(day-3) or few cells(day-5) embryo biopsy in 2.5 ul transport medium available in the Med | Sanger Sequencing |
| POC all trimester+ FISH (7 probes) | Prenatal | 15 working days | Not Available | Product of Conception(POC) | Tissue in sterile container in saline or Cardiac/Cord blood in sodium heparin vacutainer. Please add | 20-25℃,do not freeze the sample | 10 to 30 mg of clean tissue in sterile container in salineCardiac/Cord blood-2ml in sodium heparin | Cytogenetics/Karyotyping + FISH |
| POC-1st trimester | Prenatal | 15 working days | Not Available | Product of Conception(POC) | Tissue in sterile container in saline. Please add antibiotics (1-2 drops after collection) | 20-25℃,do not freeze the sample | 10 to 30 mg of clean tissue in sterile container in saline | Cytogenetics/Karyotyping |
| POC-2nd and 3rd trimester cord / cardiac blood | Prenatal | 15 working days | Not Available | Product of Conception(POC) | Tissue in sterile container in saline or Cardiac/Cord blood in sodium heparin vacutainer. Please add | 20-25℃,do not freeze the sample | 10 to 30 mg of clean tissue in sterile container in salineCardiac/Cord blood-2ml in sodium heparin | Cytogenetics/Karyotyping |
| POC-2nd trimester | Prenatal | 15 working days | Not Available | Product of Conception(POC) | Tissue in sterile container in saline or Cardiac/Cord blood in sodium heparin vacutainer. Please add | 20-25℃,do not freeze the sample | 10 to 30 mg of clean tissue in sterile container in salineCardiac/Cord blood-2ml in sodium heparin | Cytogenetics/Karyotyping |
| Pre-Implantation Genetic Screening(PGS) | Prenatal | 7 working days | Screens for aneuploidies of all 24 chromosome types including the two sex chromosomes(X and Y) and the 22 other non-sex chromosomes | Day-3 (single cell) or day-5 (few cells) embryo biopsy Note: Day-5 biopsy is preferred | 0.2 ml PCR Tubes from the PGS Kit provided by Lab. Note: Please request for the PGS kit before | -20 to -80℃ (dry ice shipment). Please contact with the Lab prior to performing the biopsy. | Single cell(day-3) or few cells(day-5) embryo biopsy in 2.5 ul transport medium available in the Med | Next Generation Sequencing |
| Pre-PGD by Sanger/PCR (1 variant) - Prospective parents and one affected kid of the couple (if available) | Prenatal | 21 working days | All 3 samples(when available) or at least the samples of prospective parents will be processed for pre PGD workup | Peripheral blood | EDTA anticoagulated peripheral blood | 20-25℃ | Minimum 3ml of peripheral blood | Sanger sequencing |
| Pre-PGD by Sanger/PCR (2 variant) - Prospective parents and one affected kid of the couple (if available) | Prenatal | 21 working days | All 3 samples(when available) or at least the samples of prospective parents will be processed for pre PGD workup | Peripheral blood | EDTA anticoagulated peripheral blood | 20-25℃ | Minimum 3ml of peripheral blood | Sanger Sequencing |
| Pre-PGD by Sanger/PCR (3 variants) - Prospective parents and one affected kid of the couple (if available) | Prenatal | 21 working days | All 3 samples(when available) or at least the samples of prospective parents will be processed for pre PGD workup | Peripheral blood | EDTA anticoagulated peripheral blood | 20-25 ℃ | Minimum 3ml of peripheral blood | Sanger Sequencing |
| Pre-PGD by Sanger/PCR (4 variants) - Prospective parents and one affected kid of the couple(if available) | Prenatal | 21 working days | All 3 samples(when available) or at least the samples of prospective parents will be processed for pre PGD workup | Peripheral blood | EDTA anticoagulated peripheral blood | 20-25 ℃ | Minimum 3ml of peripheral blood | Sanger Sequencing |
| FISH for Williams syndrome | Prenatal/Postnatal | 9 working days | Not Available | Peripheral Blood | Sodium heparin-Green top | 20-25℃ | Minimum 4 ml peripheral blood | FISH |
| High Resolution Banding [HRB] | Prenatal/Postnatal | 15 working days | Not Available | Peripheral Blood | Sodium heparin-Green top | 20-25℃ | Minimum 4 ml peripheral blood | Cytogenetics/Karyotyping |
| Prader-Willi/ Angelman syndrome by FISH | Prenatal/Postnatal | 9 working days | Not Available | Peripheral Blood | Sodium heparin-Green top | 20-25℃ | Minimum 4 ml peripheral blood | FISH |
| Newborn screening gene panel | Rare inherited diseases | 21 working days | ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL,ACAT1, ACSF3, ADA, AHCY, AK2, ARG1, ASL, ASS1, AUH, BCKDHA, BCKDHB, BTD, CBS, CD320, CD3D, CD3E, CFTR, CIITA, CPS1, CPT1A, CPT2, CYP11B1, CYP17A1, CYP21A2, DBT, DCLRE1C, DLD, DNAJC19, DUOX2, ETFA, ETFB, ETFDH, FAH, G6PD, GAA, GALC, GALE, GALK1, GALT, GBA, GCDH, GCH1, GJB2, GJB3, GJB6, GLA, GNMT, GSS, HADH, HADHA, HADHB, HBA1, HBB, HCFC1, HLCS, HMGCL, HPD, HSD17B10, HSD3B2, IDUA, IL2, IL21R, IL2RG, IL7R, IVD, JAK3, LMBRD1, MAT1A, MCCC1, MCCC2, MCEE, MLYCD, MMAA, MMAB,MMACHC, MMADHC, MTHFR, MTR, MTRR, MUT, NADK2,NGLY1, NHEJ1, NKX2, NPC1, NPC2, OAT, OPA3, OTC, PAH, PAX8, PCBD1, PCCA, PCCB, PNP, PSAP, PTPRC, PTS, QDPR, RAG1, RAG2, RFX5, RFXANK, RFXAP, SLC22A5, SLC25A13, SLC25A15, SLC25A20, SLC5A5, SMPD1, STAR, SUCLA2, SUCLG1, TAP1, TAPBP, TAT, TG, THRA, TPO, TSHB, TSHR | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Aneuploidy MLPA | Rare inherited disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Bardet-Biedl syndrome gene panel | Rare inherited disorders | 21 working days | ARL6, BBIP1, BBS1, BBS10, BBS12, BBS2, BBS4, BBS5, BBS7, BBS9, CCDC28B, CEP290, IFT27, IFT74, LZTFL1, MKKS, MKS1, SDCCAG8, TMEM67, TRIM32, TTC8, WDPCP | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Beckwith-Wiedemann syndrome deletion/duplication analysis | Rare inherited disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | MLPA |
| Blooms syndrome | Rare Inherited Disorders | 15 working days | Not Available | Peripheral Blood | Sodium heparin-Green top | 20-25℃ | Minimum 4 ml peripheral blood | Cytogenetics/Karyotyping |
| Ciliopathy gene panel | Rare inherited disorders | 21 working days | AHI1, ALMS1, ANKS6, ARL13B, ARL6, ARMC4, B9D1, B9D2, BBIP1, BBS1, BBS10, BBS12, BBS2, BBS4, BBS5, BBS7, BBS9, C21ORF59, C2CD3, C5orf42, CC2D2A, CCDC103, CCDC114, CCDC151, CCDC28B, CCDC39, CCDC40, CCDC65, CCNO, CEP120, CEP164, CEP290, CEP41, CEP83, CSPP1, DCDC2, DDX59, DNAAF1, DNAAF2, DNAAF3, DNAAF5, DNAH11, DNAH5, DNAI1, DNAI2, DNAL1, DRC1, DYNC2H1, DYX1C1, EVC, EVC2, GLIS2, HYDIN, IFT122, IFT140, IFT172, IFT27, IFT43, IFT80, INPP5E, INVS, IQCB1, KIAA0586, KIAA0753, KIF14, KIF7, LAMA1, LRRC6, LZTFL1, MKKS, MKS1, NEK1, NEK8, NME8, NPHP1, NPHP3, NPHP4, OFD1, PDE6D, PIEZO2, PKD1, PKD2, PKHD1, RPGRIP1L, RSPH1, RSPH3, RSPH4A, RSPH9, SDCCAG8, SPAG1, TCTN1, TCTN2, TCTN3, TMEM138, TMEM216, TMEM231, TMEM237, TMEM67, TRIM32, TTC21B, TTC8, WDPCP, WDR19, WDR34, WDR35, WDR60, XPNPEP3, ZMYND10, ZNF423 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Cockayne syndrome gene panel | Rare inherited disorders | 21 working days | ERCC3, ERCC4, ERCC5, ERCC6, ERCC8 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Cohen's syndrome (VPS13B) gene analysis | Rare inherited disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Cornelia de Lange syndrome gene panel | Rare inherited disorders | 21 working days | HDAC8, NIPBL, RAD21, SMC1A, SMC3 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Craniosynostosis gene panel | Rare inherited disorders | 21 working days | ALX4, CD96, CYP26B1, ERF, FGFR1, FGFR2, FGFR3, IL11RA, MEGF8, MSX2, P4HB, RAB23, RECQL4, SEC24D, SKI, SMAD3, SMAD6, TCF12, TGFB2, TGFB3, TGFBR1, TGFBR2, TWIST1, ZIC1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Cystic fibrosis (CFTR) del508 mutation analysis | Rare inherited disorders | 7 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Sanger sequencing |
| Cystic fibrosis (CFTR) gene analysis | Rare inherited disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Cystic fibrosis (CFTR) gene panel deletion/duplication analysis | Rare inherited disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Fraser syndrome gene panel | Rare inherited disorders | 21 working days | FRAS1, FREM2, GRIP1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Johanson-Blizzard syndrome (UBR1) gene analysis | Rare inherited disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Klippel-Feil syndrome gene panel | Rare inherited disorders | 21 working days | GDF3, GDF6, MEDX1, MYO18B | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| MLPA for common microdeletion syndromes | Rare inherited disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Non-immune hydrops gene panel | Rare inherited disorders | 21 working days | ALG1, ASAH1, CANT1, DHCR7, FOXC2, GALNS, GBA, GBE1, GLA, GLB1, GM2A, GNPTAB, GUSB, IDUA, LBR, LIPA, NEU1, NPC1, NPC2, PEX1, PEX10, PEX12, PEX13, PEX14, PEX16, PEX19, PEX26, PEX3, PEX5, PEX6, PMM2, PSAP, SLC17A5, SMPD1, SUMF1, UROS | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Noonan syndrome gene panel | Rare inherited disorders | 21 working days | BRAF, CBL, KRAS, LZTR1, NF1, NRAS, PTPN11, RAF1, RIT1, SHOC2, SOS1, SOS2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| PDGFRB gene sequencing | Rare inherited disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| POLG gene sequencing | Rare inherited disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Prader-Willi/Angelman syndrome deletion/duplication analysis | Rare inherited disorders | 14 working days | semi-quantitative detection of CNV and aberrant methylation in the 15q11 region. | Peripheral blood/purified genomic DNA | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | MLPA |
| Pulmonary alveolar microlithiasis (SLC34A2) gene analysis | Rare inherited disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Pulmonary surfactant metabolism dysfunction gene panel | Rare inherited disorders | 21 working days | ABCA3, CSF2RA, CSF2RB, SFTPB, SFTPC | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Rasopathy gene panel | Rare inherited disorders | 21 working days | A2ML1, BRAF, CABIN1, CBL, HRAS, KAT6B, KRAS, LZTR1, MAP2K1, MAP2K2, NF1, NF2, NRAS, NSUN2, PTPN11, RAF1, RASA2, RIT1, RRAS, SHOC2, SOS1, SOS2, SPRED1 Note: Due to the presence of pseudogenes in many of these genes, Sanger validation of variants is highly recommended. | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Seckel syndrome gene panel | Rare inherited disorders | 21 working days | ATR, CENPJ, CEP152, CEP63, DNA2, NIN, NSMCE2, RBBP8 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Smith-Lemli-Opitz syndrome (DHCR7) gene analysis | Rare inherited disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Sotos syndrome (NSD1) deletion/duplication analysis | Rare inherited disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Sotos syndrome gene panel | Rare inherited disorders | 21 working days | APC2, NFIX, NSD1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Subtelomere deletion/duplication analysis | Rare inherited disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| TTN gene sequencing | Rare inherited disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| WAGR syndrome (PAX6) deletion/duplication analysis | Rare inherited disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Achondroplasia (FGFR3) gene analysis | Skeletal dysplasia | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hereditary multiple exostoses gene panel | Skeletal dysplasia | 21 working days | EXT1 and EXT2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Osteogenesis imperfecta gene panel | Skeletal dysplasia | 21 working days | ALPL, BMP1, COL1A1, COL1A2, CRTAP, FKBP10, IFITM5, LRP5, P3H1, PLOD2, PPIB, SERPINF1, SERPINH1, SP7, SPARC, TMEM38B, WNT1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Osteopetrosis gene panel | Skeletal dysplasia | 21 working days | CA2, CLCN7, CTSK, LRP5, OSTM1, PLEKHM1, SNX10, TCIRG1, TNFRSF11A, TNFSF11 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Pachydermoperiostosis & primary hypertrophic osteoarthropathy gene panel | Skeletal dysplasia | 21 working days | HPGD, SLCO2A1 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Skeletal dysplasia gene panel | Skeletal dysplasia | 21 working days | ACAN, ACP5, ACVR1, ADAMTS1, ADAMTSL2, AGPS, ALPL, ALX3, ALX4, AMER1, ANKH, ANO5, AP2S1, ARHGAP31, ARSE, ATP6VA2, ATR, B3GALT6, B4GALT7, BHLHA9, BMP1, BMP2, BMPER, BMPR1B, CA2, CANT1, CASR, CC2D2A, CCDC8, CDC6, CDH3, CDKN1C, CDT1, CENPJ, CEP152, CEP29, CEP63, CHST14, CHST3, CHSY1, CLCN5, CLCN7, COL1A1, COL11A1, COL11A2, COL1A1, COL1A2, COL2A1, COL9A1, COL9A2, COL9A3, COMP, CREBBP, CRTAP, CTSK, CUL7, CYP27B1, CYP2R1, DDR2, DHCR24, DHCR7, DLL3, DLX3, DMP1, DNA2, DVL1, DVL3, DYM, DYNC2H1, EBP, EFNB1, EIF2AK3, ENPP1, EP3, ERF, ESCO2, EVC, EVC2, EXT1, EXT2, EZH2, FAM111A, FAM2C, FAM58A, FBLN1, FBN1, FERMT3, FGF1, FGF16, FGF23, FGF9, FGFR1, FGFR2, FGFR3, FKBP1, FLNA, FLNB, FREM1, GALNT3, GDF3, GDF5, GDF6, GJA1, GLI3, GNA11, GNAS, GNPAT, GORAB, GPC6, GSC, HDAC4, HES7, HOXA11, HOXD13, HPGD, HSPG2, IARS2, ICK, IFITM5, IFT122, IFT14, IFT172, IFT43, IFT8, IHH, IL11RA, IMPAD1, INPPL1, KIF22, KIF7, LARP7, LBR, LEMD3, P3H1, LFNG, LIFR, LMBR1, LMNA, LMX1B, LRP4, LRP5, MAFB, MATN3, MEGF8, MEOX1, MESP2, MGP, MKS1, MMP13, MMP2, MMP9, MSX2, MTAP, MYCN, NEK1, NFIX, NIN, NIPBL, NKX3-2, NOG, NOTCH2, NPR2, NSDHL, OBSL1, OFD1, ORC1, ORC4, ORC6, OSTM1, PAPSS2, PCNT, PCYT1A, PDE4D, PEX7, PHEX, PIGV, PITX1, PLEKHM1, PLOD2, PLS3, POC1A, POR, PPIB, PRKAR1A, PTDSS1, PTH1R, PTHLH, PTPN11, PYCR1, RAB23, RAB33B, RASGRP2, RBBP8, RECQL4, RMRP, RNU4ATAC, ROR2, RPGRIP1L, RUNX2, SALL1, SALL4, SBDS, SERPINF1, SERPINH1, SF3B4, SH3PXD2B, SHH, SHOX, SKI, SLC25A12, SLC26A2, SLC34A1, SLC34A3, SLC35D1, SLC39A13, SLC9A3R1, SLCO2A1, SMARCAL1, SNX1, SOST, SOX9, SP7, SPARC, TBCE, TBX15, TBX3, TBX4, TBX5, TBX6, TBXAS1, TCF12, TCIRG1, TCTN3, TGFB1, THPO, TMEM216, TMEM38B, TMEM67, TNFRSF11A, TNFRSF11B, TNFSF11, TP63, TRAPPC2, TREM2, TRIP11, TRPS1, TRPV4, TTC21B, TWIST1, TYROBP, VDR, WDR19, WDR34, WDR35, WDR6, WISP3, WNT1, WNT1B, WNT3, WNT5A, WNT7A, XYLT1, ZMPSTE24, ZSWIM6 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Aneuploidy by QF PCR [with MCC] | Additional options for testing | 4 working days | Not Available | Either amniotic fluid/chorionic villus sample (CVS) /Product of conception or the purified genomic D | Amniotic fluid in a sterile falcon tube/cultured cells CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic Tissue in sterile container in saline or Cardiac/Cord blood in sodium heparin vacutainer. Please add antibiotic(1-2 drops after collection)/DNA in sealed Eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters) | Fragment analysis |
| Chromosomal Microarray - Affymetrix Cytoscan 750K genechip | Additional options for testing | 12 working days | 750000 CNV/200000 genotypable probes. The array contains 550,000 unique non-polymorphic probes and approximately 200,000 genotype-able SNPs Primary indications: 1) Unexplained developmental delay (DD) 2) Intellectual disability(ID)or mental impairment 3) Autism spectrum disorders (ASD) 4) Multiple congenital anomalies (MCA) | Peripheral blood/Purified genomic DNA/Chorionic villus sample (CVS)/Amniotic fluid (AF)/Product of Conception | Peripheral Blood : EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; Purified genomic DNA | Peripheral Blood : 20-25℃; Purified genomic DNA : 2-8℃; Chorionic villus sample (CVS) : 2-8℃; Amniotic fluid: 20-25℃; POC: 20-25℃ | Peripheral Blood : Minimum 3ml of peripheral blood. Purified genomic DNA : minimum 1 microgram of DNA | Microarray |
| Chromosomal Microarray - Affymetrix Cytoscan HD genechip | Additional options for testing | 12 working days | HD Array includes 2.67 million markers for copy number (CN) analysis, including 750,000 biallelic SN | Peripheral blood/Purified genomic DNA/Chorionic villus sample (CVS)/Amniotic fluid (AF)/Product of Conception | Peripheral Blood : EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; Purified genomic DNA | Peripheral Blood : 20-25℃; Purified genomic DNA : 2-8℃; Chorionic villus sample (CVS) : 2-8℃; Amniotic fluid: 20-25℃; POC: 20-25℃ | Peripheral Blood : Minimum 3ml of peripheral bloodPurified genomic DNA : minimum 1 microgram of DNA | Microarray |
| Chromosomal Microarray - Affymetrix Cytoscan Optima low resolution genechip | Additional options for testing | 12 working days | 8,018 CNV probes and 148,450 SNP markers**uniformly spaced over the genome with enhanced interrogation of 396 regions of prenatal interest1. A minimum resolution of 1 MB for losses,2 MB for gains, and 5 MB for LOH/AOH2. Increased coverage density(25 markers/100 kb) in 396 empirically selected regions relevant for prenatal research | Peripheral blood/Purified genomic DNA/Chorionic villus sample (CVS)/Amniotic fluid (AF)/Product of Conception | Peripheral Blood : EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; Purified genomic DNA | Peripheral Blood : 20-25℃; Purified genomic DNA : 2-8℃; Chorionic villus sample (CVS) : 2-8℃; Amniotic fluid: 20-25℃; POC: 20-25℃ | Peripheral Blood : Minimum 3ml of peripheral blood; Purified genomic DNA : minimum 1 microgram of DNA | Microarray |
| Clinical exome - 26MB(80-100x) | Additional options for testing | 21 working days | 8332 genes. Coverage list may be provided separately | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Clinical exome - 26MB(80-100x) - [ONLY RAW DATA, NO CLINICAL REPORT] | Additional options for testing | 21 working days | 8332 genes. | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Clinical Exome with reflex Sanger for investigational - 26MB (80-100x) | Additional options for testing | 28 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing & Sanger |
| CMA XON Array | Additional Options for Testing | 14 working days | CytoScan XON Array consists of approximately 6.85M probes of which 6.55M are non-polymorphic copy number probes and approximately 300,000 are SNP markers. It is designed to cover the whole genome, with an increased focus on 7,000 clinically relevant genes at exon level. | Peripheral blood/Purified genomic DNA/Chorionic villus sample (CVS)/Amniotic fluid (AF)/Product of C | Peripheral Blood : EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tubePurified genom | Peripheral Blood : 20-25℃Chorionic villus sample (CVS) : 2-8℃Amniotic fl | Peripheral Blood : Minimum 3ml of peripheral bloodPurified genomic DNA : minimum 1 microgram of DNA | Microarray |
| DNA Extraction and Storage | Additional Options for Testing | 4 working days | The time period for the storage of DNA is 6 months | Peripheral blood/Direct DNA | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube | 20-25℃ | Minimum 3ml of peripheral blood/Minimum 1 ?g of DNA suspended in TE buffer | DNA Extraction |
| FISH for SRY | Additional Options for Testing | 7 working days | Not Available | Peripheral Blood | Sodium heparin-Green top | 20-25℃ | Minimum 3 ml peripheral blood | FISH |
| Karyotyping (Non-Leukemia) | Additional Options for Testing | 15 working days | Not Available | Peripheral Blood | Sodium heparin-Green top | 20-25℃ | Minimum 4 ml peripheral blood | Cytogenetics/Karyotyping |
| Maternal Cell Contamination (MCC) check in prenatal DNA | Additional options for testing | 7 working days | Not Available | Either amniotic fluid/chorionic villus sample (CVS) /Product of conception or the purified genomic D | Amniotic fluid in a sterile falcon tube/cultured cells CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic Tissue in sterile container in saline or Cardiac/Cord blood in sodium heparin vacutainer. Please add antibiotic(1-2 drops after collection)/DNA in sealed Eppendorf tube | 20-25℃ CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency | Fragment analysis |
| MLPA for mitochondrial DNA | Additional options for testing | 14 working days | Not Available | Peripheral blood/purified genomic DNA (RNAse treated)/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Prenatal sanger variant analysis [1 variant] | Additional Options for Testing | 28 working days | Detailed clinical and family history is mandatory for processing this test | Chorionic villus sample (CVS)/amniotic fluid/fetal DNA | CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic;Amniotic fluid in a sterile f | 20-25℃CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency; minimum 1 microg | Sanger sequencing |
| Prenatal sanger variant analysis [2 variants] | Additional Options for Testing | 28 working days | Detailed clinical and family history is mandatory for processing this test | Chorionic villus sample (CVS)/amniotic fluid/fetal DNA | CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic;Amniotic fluid in a sterile f | 20-25℃CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency; minimum 1 microg | Sanger sequencing |
| Sanger validation [1 variant] | Additional options for testing | 28 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Sanger sequencing |
| Sanger validation [2 variants] | Additional options for testing | 28 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Sanger sequencing |
| Sperm FISH (5 Probes - 13,18,21,X,Y) | Additional Options for Testing | 4 working days | Not Available | Semen | 4 semen slides (Air dried packed face to face) or 1ml semen sample | 20-25℃,do not freeze the sample | 4 semen slides (Air dried packed face to face) or 1ml semen sample | FISH |
| TRIO - Whole exome sequencing SureSelectV5 50MB (80-100x) | Additional options for testing | 28 working days | All 3 samples will be processed for whole exome sequencing simultaneously | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| TRIO Clinical Exome sequencing - 26MB (80-100x) | Additional options for testing | 21 working days | All 3 samples will be processed for clinical exome sequencing simultaneously. Clinical exome consists of 8332 genes. Coverage list may be provided separately | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Whole exome sequencing SureSelectV5 - 50MB (80-100x) | Additional options for testing | 21 working days | Detailed clinical and family history is mandatory for processing this test | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Whole genome sequencing (mean 10x) | Additional options for testing | 56 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Whole genome sequencing (mean 30x) | Additional options for testing | 56 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Whole mitochondrial genome sequencing | Additional options for testing | 14 working days | Detailed clinical and family history is mandatory for processing this test. Genes : ATP6, ATP8, COX1, COX2, COX3, CYTB, ND1, ND2, ND3, ND4, ND4L, ND5, ND6, RNR1, RNR2, TRNA, TRNC, TRND, TRNE, TRNF, TRNG, TRNH, TRNI, TRNK, TRNL1, TRNL2, TRNM, TRNN, TRNP, TRNQ, TRNR, TRNS1, TRNS2, TRNT, TRNV, TRNW, TRNY | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Amniocentesis / CVS Culturing + DNA Extraction & Storage | Additional Options for Testing | 16 working days | Not Available | Amniotic Fluid/ Chorionic Villus Sample (CVS) | Amniotic fluid in 2 sterile falcon tubes/ CVS In a sterile 15ml falcon tube in provided medium | 20-25℃ | 2 tubes with 10ml in each sterile tube/ CVS 20 - 30mg | Cytogenetics/Karyotyping |
| AFB DIRECT SMEAR/CONC METHOD | Infectious Disease | 1 working day | Not Available | Sputum/Extra Pulmonary (EP) samples | Sterile Container | 2-8℃ | 1- 2 ml | Others |
| Atypical identification test | Infectious Disease | 4 working days | If Sputum or other specimens are received then Additional Test (MGM1634) will be performed with the charges applicable | Culture | Culture in Media | 2-8℃ | NA | Others |
| Sensitivity for Atypical mycobacterium | Infectious Disease | 28 working days | On Request | Culture | Culture in Media | 2-8℃ | NA | Others |
| XPERT MTB-RIF Assay (for Sputum) | Infectious Disease | 1 working day | Blood not acceptable | Sputum/Extra Pulmonary (EP) samples | Sterile Container | 2-8℃ | 1- 2 ml | Others |
| XPERT MTB-RIF Assay (for Tissue) | Infectious Disease | 1 working day | Blood not acceptable | Sputum/EP Samples | Sterile Container | 2-8℃ | 1- 2 ml | Others |
| LINE PROBE ASSAY 1ST LINE Drugs | Infectious Disease | 4 working days | Not Available | Culture Isolates/Sputum/Extra Pulmonary (EP) samples | Sterile Container | 2-8℃ | 1- 2 ml | Others |
| LINE PROBE ASSAY 2nd LINE Drugs | Infectious Disease | 4 working days | Not Available | Culture Isolates/Sputum/Extra Pulmonary (EP) samples | Sterile Container | 2-8℃ | 1- 2 ml | Others |
| COVID-19 (SARS-CoV2) RT-PCR test | Infectious Disease | 2 working days | Both Nasopharyngeal and Oropharyngeal Swab of the same patient has to be collected in the same VTM tube | Nasopharyngeal and Oropharyngeal Swab/Bronchoalveolar Lavage (BAL) / Endotracheal Aspirate/Sputum | Swabs collected in Viral Transport Medium (VTM) | 2-8℃ | NA | RT-PCR |
| Bartter syndrome gene panel | Nephrology | 21 working days | BSND, CASR, CLCNKA, CLCNKB, KCNJ1, MAGED2, SLC12A1, SLC12A3 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; Amniotic fluid in a sterile falcon tube/cultured cells | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| RAS Extended profiling analysis by NGS | Oncology | 12 working days | HOTSPOT Mutations in: Exon 2, 3 & 4 of KRAS gene ; Exon 2, 3 & 4 of NRAS gene ; Exon 15 of BRAF gene For theranostic monitoring of colorectal cancers | FFPE blocks | Cardboard box | 20-25℃ | Minimum 10% (as assessed by the pathologist) of tumor tissue should be available | Next Generation Sequencing |
| AF Cell Culture (Amniotic fluid only) with Clinical Exome - 26MB (80-100x) | Prenatal | 33 working days | Not Available | Amniotic Fluid | Amniotic fluid in 2 sterile falcon tubes | 20-25℃ | 2 tubes with 10ml in each sterile tube | Cytogenetics/Karyotyping |
| AF Cell Culture (Amniotic fluid only) | Prenatal | 12 working days | Not Available | Amniotic Fluid | Amniotic fluid in 2 sterile falcon tubes | 20-25℃ | 2 tubes with 10ml in each sterile tube | Cytogenetics/Karyotyping |
| AF Cell Culture (Amniotic fluid only) with Chromosomal Microarray - Affymetrix Cytoscan 750K Genechip | Prenatal | 24 working days | Not Available | Amniotic Fluid | Amniotic fluid in 2 sterile falcon tubes | 20-25℃ | 2 tubes with 10ml in each sterile tube | Cytogenetics/Karyotyping |
| AF Cell Culture (Amniotic fluid only) with Chromosomal Microarray - Affymetrix Cytoscan Optima low resolution Genechip | Prenatal | 24 working days | Not Available | Amniotic Fluid | Amniotic fluid in 2 sterile falcon tubes | 20-25℃ | 2 tubes with 10ml in each sterile tube | Cytogenetics/Karyotyping |
| AF Cell Culture (Amniotic fluid only) with Sanger variant analysis [1 variant] | Prenatal | 40 working days | Not Available | Amniotic Fluid | Amniotic fluid in 2 sterile falcon tubes | 20-25℃ | 2 tubes with 10ml in each sterile tube | Cytogenetics/Karyotyping |
| AF Cell Culture (Amniotic fluid only) with Sanger variant analysis [primers available] - 1 variant | Prenatal | 24 working days | Not Available | Amniotic Fluid | Amniotic fluid in 2 sterile falcon tubes | 20-25℃ | 2 tubes with 10ml in each sterile tube | Cytogenetics/Karyotyping |
| MCC [REFLEX] with Clinical Exome - 26MB (80-100x) | Prenatal | 28 working days | Not Available | Either amniotic fluid/chorionic villus sample (CVS) /Product of conception or the purified genomic DNA extracted from either of these | Amniotic fluid in a sterile falcon tube/cultured cells CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic Tissue in sterile container in saline or Cardiac/Cord blood in sodium heparin vacutainer. Please add antibiotic(1-2 drops after collection)/DNA in sealed Eppendorf tube | 20-25℃ CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency | Fragment analysis |
| MCC [REFLEX] with Chromosomal Microarray - Affymetrix Cytoscan 750K Genechip | Prenatal | 14 working days | Not Available | Either amniotic fluid/chorionic villus sample (CVS) /Product of conception or the purified genomic DNA extracted from either of these | Amniotic fluid in a sterile falcon tube/cultured cells CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic Tissue in sterile container in saline or Cardiac/Cord blood in sodium heparin vacutainer. Please add antibiotic(1-2 drops after collection)/DNA in sealed Eppendorf tube | 20-25℃ CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency | Fragment analysis |
| MCC [REFLEX] with Chromosomal Microarray - Affymetrix Cytoscan Optima low resolution Genechip | Prenatal | 19 working days | Not Available | Either amniotic fluid/chorionic villus sample (CVS) /Product of conception or the purified genomic DNA extracted from either of these | Amniotic fluid in a sterile falcon tube/cultured cells CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic Tissue in sterile container in saline or Cardiac/Cord blood in sodium heparin vacutainer. Please add antibiotic(1-2 drops after collection)/DNA in sealed Eppendorf tube | AF at 20-25℃; CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency | Fragment analysis |
| MCC [REFLEX] with Prenatal sanger variant analysis [1 variant] | Prenatal | 35 working days | Not Available | Either amniotic fluid/chorionic villus sample (CVS) /Product of conception or the purified genomic DNA extracted from either of these | Amniotic fluid in a sterile falcon tube/cultured cells CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic Tissue in sterile container in saline or Cardiac/Cord blood in sodium heparin vacutainer. Please add antibiotic(1-2 drops after collection)/DNA in sealed Eppendorf tube | AF at 20-25℃; CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency | Fragment analysis |
| MCC [REFLEX] Prenatal sanger variant analysis [Primers available] - 1 variant | Prenatal | 19 working days | Not Available | Either amniotic fluid/chorionic villus sample (CVS) /Product of conception or the purified genomic DNA extracted from either of these | Amniotic fluid in a sterile falcon tube/cultured cells CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic Tissue in sterile container in saline or Cardiac/Cord blood in sodium heparin vacutainer. Please add antibiotic(1-2 drops after collection)/DNA in sealed Eppendorf tube | AF at 20-25℃; CVS at 2-8℃ | 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency | Fragment analysis |
| Cantu syndrome (ABCC9) gene sequencing | Rare inherited disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid/ Dried Blood Spots (FTA Cards)/ Product of Conception (POC) | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon tube/cultured cells; CVS in a sterile 15ml falcon tube with RPMI1640+10% FBS+ 1% antibiotic ; For Product of conception(POC) - Wide mouth screw capped containers with plain RPMI, or sterile saline may be used for transportation of the specimen | AF at 20-25℃; CVS at 2-8℃; POC at 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); 300-500mg of CVS; Amniotic fluid of 15-20ml/T25 culture flask with 100% confluency For Dried Blood Spots (FTA Cards) - Maximum 125 µl of the sample to be spotted per area of the card. Five full blood spots (circles) are required in order to run the test For Product of Conception (POC) - Fresh placental or fetal tissue(Min: 5 mg) submerged in stable transport media or sterile saline 1.In case of autopsy- skin or tissue from internal organs (if fresh) or placenta from fetal side. 2.If no autopsy is performed: Placenta from fetal side is preferred (e.g. villi) 3.n case of Placenta, maternal cell contamination to be ruled out. Maternal blood sample to be sent along for MCC testing Should NOT FREEZE. Should NOT be placed in formalin | Next Generation Sequencing |
| Kardiogen Test (CAD -PRS) | Cardiology | 12 working days | 6.6 Million genomic Markers responsible for CAD development | Blood | EDTA vacutainer | 2-8℃ | minimum of 3 ml whole blood | DNA genotyping Array |
| SES Uveitis | Eye Infection panels | 1 working day | Mycobacterium tuberculosis; Mycobacterium chelonae; Mycobacterium fortuitum; Toxoplasma gondii | Aqueous Humor/Vitreous aspirate, Vitreous lavage, Any other eye specimen | Sample collected in 1ml insulin syringe - Potassium EDTA vacutainer (Kit provided by the company) | Room temperature | 100 uL | PCR |
| Congenital amegakaryocytic thrombocytopenia (MPL) gene analysis | Hematology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Karyotyping (Leukemia) | Hemato-Oncology | 10 working days | Not Available | Bone marrow aspirate | Sodium heparin-Green top | 20-25℃ | Minimum 2 ml of bone marrow aspirate | Cytogenetics/Karyotyping |
| Chediak-Higashi syndrome (LYST) gene analysis | Immunology | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| HLA TYPING-HR (HLA A*,B*,C*,DRB1*,DQB1* and DPB1*) | Immunology | 10 working days | Label each tube clearly with name/Age/Sex | Peripheral blood; purified genomic DNA; buccal swabs (4) for patients on chemotherapy or anemic pati | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; buccal swabs in a sterile contai | 20-25℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Peroxisomal disorder gene panel (includes adrenoleukodystrophy) | Metabolic disorders | 21 working days | ABCD1, ACOX1, AMACR, HSD17B4, PEX1, PEX10, PEX11B, PEX12, PEX13, PEX14, PEX16, PEX19, PEX2, PEX26, PEX3, PEX5, PEX6, PEX7, PHYH | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Hereditary spastic paraplegia gene panel | Neurology - Movement Disorders | 21 working days | ABCD1, ALDH18A1, ALS2, AMPD2, AP4B1, AP4E1, AP4M1, AP4S1, AP5Z1, ARL6IP1, ATL1, ATP13A2, B4GALNT1, BICD2, BSCL2, C12orf65, C19orf12, CAPN1, CCT5, CPT1C, CYP2U1, CYP7B1, DDHD1, DDHD2, ENTPD1, ERLIN1, ERLIN2, EXOSC3, FA2H, FARS2, FLRT1, GAD1, GBA, GBA2, GJC2, HSPD1, IBA57, KIAA0196, KIDINS220, KIF1A, KIF1C, KIF5A, KLC2, L1CAM, LYST, MAG, NIPA1, NT5C2, PLP1, PNPLA6, REEP1, REEP2, RTN2, SACS, SLC16A2, SLC1A4, SLC2A1, SLC33A1, SPAST, SPG11, SPG20, SPG21, SPG7, TECPR2, TFG, USP8, VAMP1, VPS37A, ZFYVE26, ZFYVE27 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Charcot-Marie-Tooth type 4C (SH3TC2) deletion/duplication analysis | Neurology - neuromuscular | 14 working days | this MLPA only partially covers SH3TC2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Myotonia congenita gene panel | Neurology - neuromuscular | 21 working days | CLCN1, SCN4A | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed eppendorf tube; amniotic fluid in a sterile falc | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| FISH for Deletion 7/7q (7q22,7q31), MDS/AML/CML/JMML | Oncology | 6 working days | Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| FISH for Leukaemia panel (4 markers) | Oncology | 7 working days | Includes MLL rearrangement, BCR/ABL t(9;22) fusion, ETV6 RUNX1 fusion and iAMP-21. Provide detailed clinical history along with bone marrow findings. All samples for FISH to reach the lab with in 24 hours of collection for best results. If Peripheral blood sample is provided, then include the Peripheral blood findings also. | Bone marrow aspirate (preferred) or peripheral blood | Sodium heparin - Green top | 20-25℃ | Minimum 1ml of bone marrow aspirate; minimum 4ml of peripheral blood | FISH |
| Microphthalmia and anophthamia gene panel | Ophthalmology | 21 working days | ABCB6, ALDH1A3, BCOR, BMP4, FRAS1, FREM2, GDF3, GDF6, GRIP1, HCCS, HDAC6, HMGB3, HMX1, MAB21L2, MFRP, MITF, NAA10, OTX2, PAX6, PRSS56, PXDN, RAB3GAP1, RARB, RAX, RBP4, SHH, SIX6, SMOC1, SOX2, STRA6, TENM3, VAX1, VCX2, VSX2 | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |
| Amniotic Fluid karyotyping only | Prenatal | 15 working days | Not Available | Amniotic Fluid | Amniotic fluid in 2 sterile falcon tubes | 20-25℃ | 2 tubes with 10ml in each sterile tube | Cytogenetics/Karyotyping |
| DiGeorge syndrome deletion/duplication analysis | Rare inherited disorders | 14 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | MLPA |
| Pallister Hall syndrome (GLI3) gene analysis | Rare inherited disorders | 21 working days | Not Available | Peripheral blood/purified genomic DNA/chorionic villus sample (CVS)/amniotic fluid | EDTA anticoagulated peripheral blood; DNA in sealed Eppendorf tube; amniotic fluid in a sterile falcon | 20-25℃ CVS at 2-8℃ | Minimum 3ml of peripheral blood; minimum 1 microgram of DNA (concentration of 50-100ng/microliters); | Next Generation Sequencing |